Etiology
- Thrombotic: Atherosclerosis, small vessel lipohyalinosis (lacunar infarcts) → fluctuating symptoms with periods of improvement
- Embolic: Afib, carotid disease, endocarditis, septal defects (PFO) → maximal severity at onset, multiple infarcts in different regions
- Hypoperfusion: Shock → global, nonspecific defects
CHA₂DS₂-VASc Score for Atrial Fibrillation Stroke Risk
Labs to Consider
- STAT fingerstick glucose
- CBC
- Electrolytes including Ca/Mg/Phos
- Liver function tests
- Coagulation studies
- Generally PT, PTT, fibrinogen
- Anti-Xa for patients on oral Xa inhibitors (e.g., apiXaban)
- Blood cultures x2 if concern for endocarditis (e.g., fever or history of IV drug use)
- Pregnancy test as appropriate
Diagnosis
CT to rule out hemorrhage (& determine tPA candidacy)
↓
MRI
↓
Source localization with duplex US (or CTA/MA), cardiac monitoring, TTE, ambulatory loop recorder
| Stroke Region | Subtype | Clinical Features |
|---|---|---|
| Cortical | Anterior Cerebral | Contralateral motor/sensory deficit, with lower extremity predominance; Behavioral changes (abulia, dyspraxia, emotional change) |
| Middle Cerebral | Contralateral motor/sensory deficit, with upper extremity and face predominance; Eye deviation towards side of infarction (frontal eye fields) | |
| Posterior Cerebral | Homonymous hemianopsia; Aphasia (dominant) or neglect (non-dominant); Possible sensory symptoms (from lateral thalamic infarct) | |
| Contralateral hemianopia with macular sparing | ||
| Brainstem | Anterior spinal | Medial Medullary Syndrome: Contralateral upper/lower limb paralysis; Ipsilateral hypoglossal (tongue deviates towards lesion); Loss of proprioception (medial lemniscus) |
| PICA | Wallenberg Syndrome (Lateral Medullary): Dysphagia/Hoarseness, Pain/temp from ipsilateral face / contralateral body, Ipsilateral Horner syndrome, Vertigo, nystagmus, ataxia, dysmetria | |
| AICA | Lateral Pontine Syndrome: Ipsilateral facial paralysis (facial nucleus); Ipsilateral pain/temp from face/contralateral body; Ipsilateral decreased lacrimation/salivation/taste from anterior tongue; Vertigo, nystagmus, ataxia, dysmetria | |
| Basilar | Medial pons, possible "Locked-In Syndrome": Corticospinal: Unilateral or bilateral paresis; Bulbar: Unilateral or bilateral face weakness, dysarthria, dysphagia, limited jaw movement; Oculomotor: Horizontal gaze palsy, internuclear ophthalmoplegia | |
| Lacunar | Pure Motor | Internal capsule (posterior limb): Unilateral paralysis of face, arm, leg without sensory loss |
| Pure Sensory | Thalamus: Unilateral sensory deficit of face, arm, leg without motor loss | |
| Ataxic Hemiparesis | Internal capsule, basis pontis, or corona radiata: Unilateral weakness and limb ataxia | |
| Dysarthria-Clumsy Hand | Genu of internal capsule, basal pons: Unilateral face weakness, dysarthria, with hand weakness and clumsiness |
Management
- Thrombolytic: IV Alteplase→ given within 3 - 4.5h (contraindications below)
- BP control (permissive htn): Labetolol, Nicardipine, and Clevidipine
- < 185/110 if tPA used
- < 220/120 if no tpa
- Aspirin (or Clopidogrel if allergic): 325mg loading dose within 48h, if tPA used do not start for 24h
- Statin: For all
- Mechanical thrombectomy: being utilized with increased frequency for proximal large vessel occlusions
Contraindications for tPA
| Major Exclusion Criteria | Relative Exclusion Criteria |
|---|---|
| Recent major surgery or trauma | History of stroke or head injury within 3 months |
| Intracranial hemorrhage or known brain tumor | Active bleeding or bleeding diathesis |
| Known intracranial structural abnormalities | Severe uncontrolled hypertension |
| Suspected aortic dissection | Recent use of anticoagulants |
| Seizure at the onset of stroke | History of gastrointestinal bleeding within 21 days |
| Rapidly improving or minor stroke symptoms | Platelet count <100,000/mm³ |
| Known severe liver disease or hepatic dysfunction | Blood glucose concentration <50 mg/dL or >400 mg/dL |
| Current use of direct thrombin inhibitors | Current use of novel oral anticoagulants |
| Pregnancy or postpartum period (within 14 days) | Dementia or severe cognitive impairment |
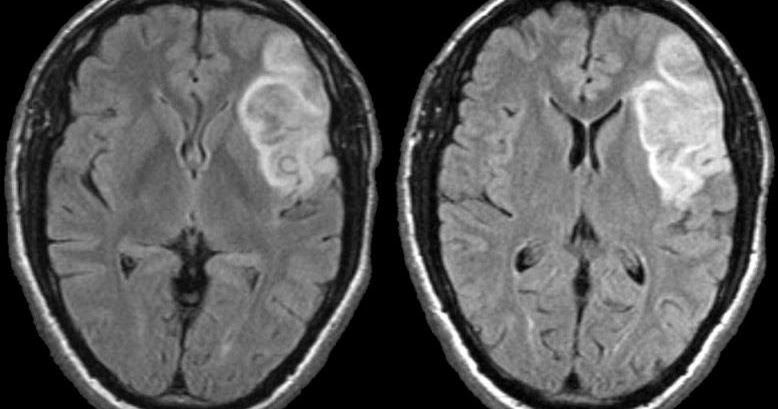
Hemorrhagic Transformation
Hemorrhagic transformation may result from the natural evolution of ischemic stroke, usually within the first week
- Petechial hemorrhages: Most hemorrhagic transformations are small, petechial hemorrhages of little clinical significance
- Asymptomatic hematomas: Small hematomas can occur within infarcted brain
- Symptomatic hematomas: Large hematomas may exert mass effect, cause vasogenic edema, and worsen clinical outcomes
Risk factors
- Large infarct size (e.g., hypodensity in more than a third of the MCA territory)
- Coagulopathy (e.g., therapeutic anticoagulation or thrombolysis)
- Older age
- Diabetes mellitus, hyperglycemia
- Uncontrolled hypertension
Treatment
- Stop thrombolytics, reverse any coagulopathies, measure coagulation labs (INR, PTT, fibrinogen, complete blood count, type & cross-match)
TIA
- TIA is a focal neurologic deficit that resolves within 24h
- Diagnose with MRI or CT
- Source localization: Duplex ultrasound, CT/ MRA, cardiac monitoring, TTE
- Management: Weight loss, smoking cessation, ASA, statin
- Stroke Risk: 8% at 30 days and 10% at 90 days
