REDUCE
Is short-term systemic corticosteroid therapy noninferior to conventional corticosteroid therapy in patients with acute exacerbation of COPD?
Study design
Population
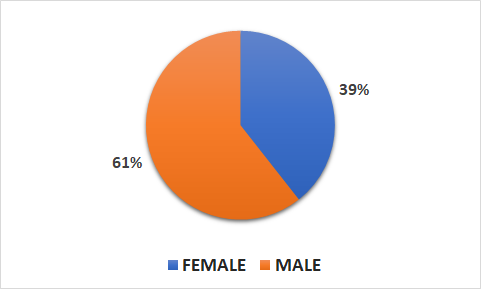
- 314 patients (123 female, 188 male)
- Inclusion criteria: patients presenting to the emergency department with acute COPD exacerbation
- Key exclusion criteria: history of asthma, ratio of FEV1 to FVC > 70% as evaluated by bedside
postbronchodilator spirometry, radiological diagnosis of pneumonia, estimated survival < 6 months due to severe comorbidity, pregnancy or lactation
Interventions
- N=156 short-term treatment (40 mg of prednisone daily for 5 days)
- N=155 conventional treatment (40 mg of prednisone daily for 14 days)
Primary outcome
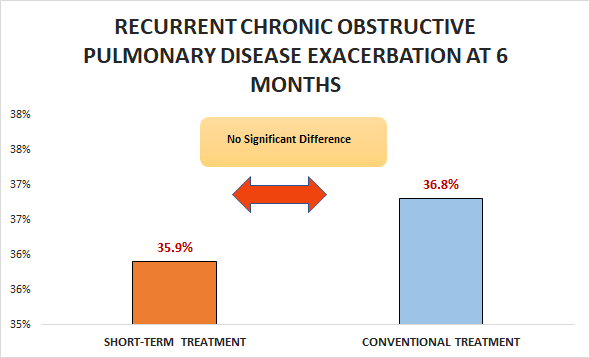
Difference not exceeding nonferiority margin in recurrent COPD exacerbation at 6 months (35.9% vs. 36.8%; HR 0.95, 95% CI 0.7 to 1.29)
Secondary outcomes
- No significant difference in need for mechanical ventilation (11% vs. 13.6%; OR 0.78, 95% CI 0.37 to 1.63)
- Significant increase in hospital stay (8 vs. 9; HR 1.25, 95% CI 0.99 to 1.59)
Safety outcomes
- No significant differences in treatment-associated adverse reactions, including hyperglycemia and HT.
- Significant differences in mean cumulative prednisone dose (379 vs. 793 mg, p < 0.001).
Conclusion
In patients presenting to the emergency department with acute COPD exacerbation, short-term treatment was noninferior to conventional treatment with respect to recurrent COPD exacerbation at 6 months.
