
Overview
- Microcytosis (small red blood cells) and hypochromasia (pale RBCs), with a mean corpuscular volume (MCV) <80 fL
- Symptoms include fatigue, weakness, pagophagia (craving ice), and dyspnea on exertion
History & Evaluation
- Assess for sources of bleeding (GI, menstrual, etc.), malabsorption (celiac disease), or a family history of anemia
- Menstrual history is crucial in reproductive-age women, as heavy bleeding is a common cause
- GI workup: Consider in men, postmenopausal women, or cases with GI symptoms or family history of colon cancer
Key Lab Findings
- Hemoglobin & MCV: Helps differentiate between IDA, thalassemia, anemia of chronic disease, and sideroblastic anemia
- Mentzer Index: MCV/RBC count. <13 suggests thalassemia, >16 suggests IDA
- Reticulocyte Count: Low (<2%) in IDA, higher in bleeding or hemolysis
- Ferritin: Best indicator of iron stores. IDA is likely if <30 mcg/L, though inflammatory states can elevate ferritin
- TIBC, Iron Saturation, RDW: Less specific but can support diagnosis
Mentzer Index Calculator
When to Treat?
- Treat if Hgb < 13 g/dL in men and < 12 g/dL in nonpregnant women
- Treat if ferritin < 45 ng/mL or TSAT <= 20%
Management
Diet & Oral Iron Therapy
- Diet: Iron from meat is better absorbed than plant sources. Avoid spinach, coffee, and tea near iron intake
- Oral Iron: Ferrous sulfate preferred (325mg EOD); alternatives include ferrous gluconate or ferrous bisglycinate
- Dosing: Once daily preferred. Alternate-day dosing may reduce GI side effects but is harder to remember
- Vitamin C: May enhance iron absorption but not always necessary
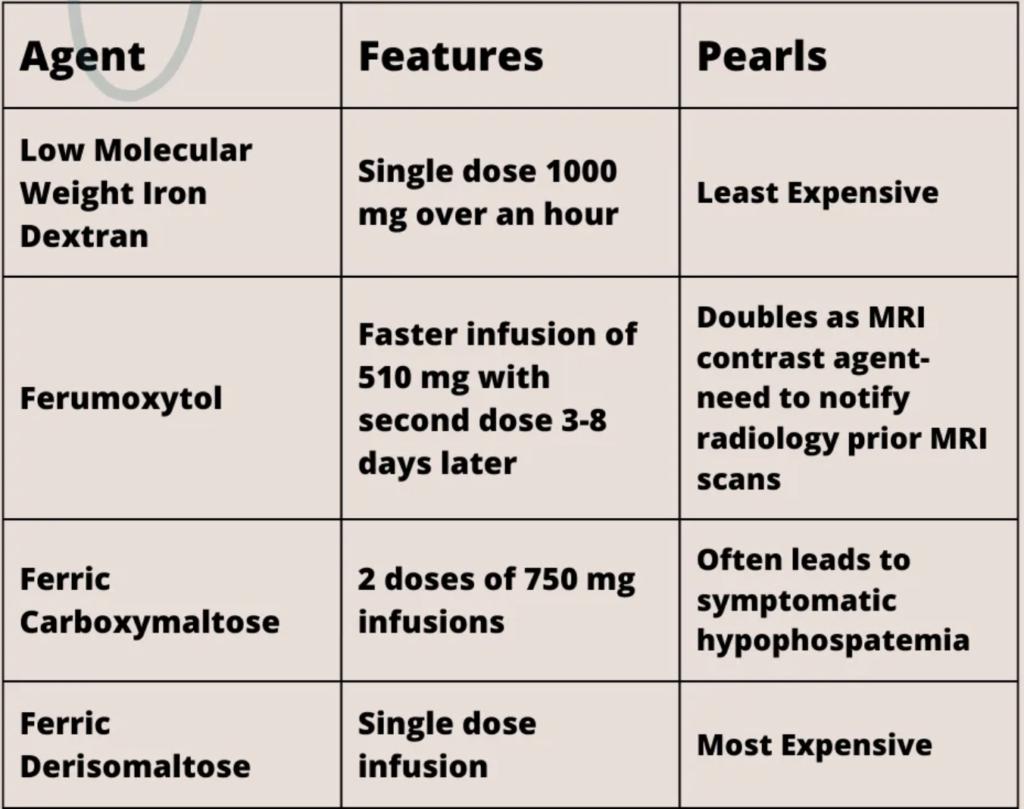
IV Iron Therapy
- Indicated for intolerance to oral iron, malabsorption (IBD, bariatric surgery), or severe deficiency
- Iron dextran: Single 1000 mg dose
- Ferumoxytol: Rapid infusion, affects MRI readings
- Ferric carboxymaltose: Risk of severe hypophosphatemia
- Ferric derisomaltose: Single-dose option
- Reactions: Usually non-IgE-mediated; premedication needed for high-risk patients
Monitoring
- Oral Iron: Check Hgb and ferritin at 3 months
- IV Iron: Check ferritin at 1 month, then every 3 months. Repeat IV iron if ferritin <50
Special Considerations
- Restless Leg Syndrome (RLS): Aim for ferritin >75 mcg/L
- Alopecia: Iron supplementation may help in iron-related hair loss
- Anemia of Chronic Disease: Often requires IV iron due to hepcidin-mediated iron sequestration
When to Refer to Hematology
- Recurrent need for IV iron
- Diagnostic uncertainty
- Associated abnormal lab findings
