Hyperkalemia

Causes: K>5.0mM
Potassium Excess
- Acute/Chronic kidney disease
- Decreased ECV
- Decreased aldosterone: type 4 RTA, adrenal insufficiency, ACEI/ARBs
- K+ sparing diuretics
Redistribution
- Diabetes, beta-blockers, metabolic/ respiratory acidosis
- Insulin deficiency, beta-adrenergic blockade, metabolic or respiratory acidosis
Lab error (Pseudohyperkalemia)
- Hemolysis
- Prolonged tourniquet use
EKG
Hyperkalemia can present with various EKG changes which may not necessarily follow a textbook sequence. It can mimic many pathologies such as STEMI and various bundle/conduction blocks. Severe hyperkalemia (Potassium >7 mM) might even occur without notable EKG changes
- Peaked T-waves: Narrow, pointy, and prominent T-waves. Often, this is the most visible finding on the EKG
- Ventricular tachycardia mimic: In this case, the QRS wave widens and P-waves might disappear, making it look like ventricular tachycardia. The T-waves could be sharper than usual, and the heart rate may be slower than expected for ventricular tachycardia
- Profound widening of QRS complex and peaked T-waves mimicking a sine wave
- Bradycardia
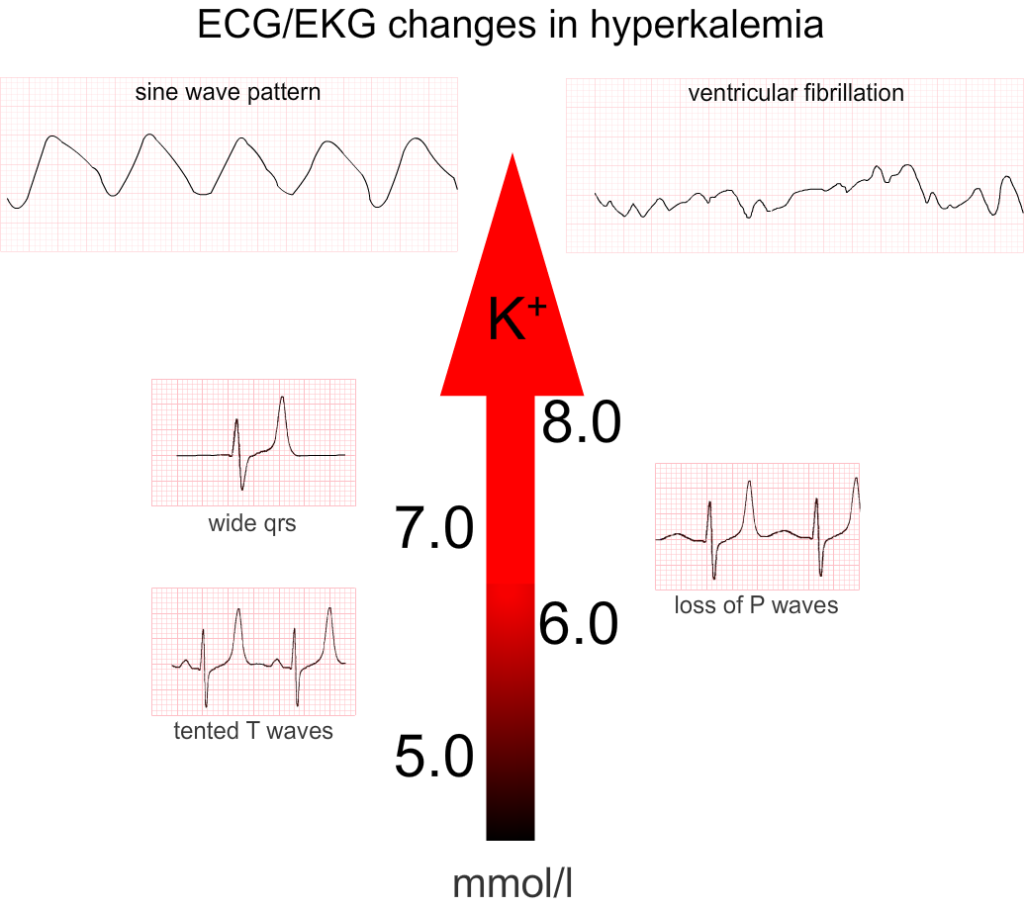
Textbook EKG progression in hyperkalemia (although this is rarely the case in real life)
Symptoms
Many patients with hyperkalemia are asymptomatic. However, if left untreated, hyperkalemia may cause: Neuromuscular weakness, bradycardia, ventricular tachycardia/fibrillation, or sudden cardiac death.
Severity & Risk Stratification
Potassium level: Levels greater than 6.5-7 mM are more worrisome
Chronicity: Chronic hyperkalemia is better tolerated than acute hyperkalemia
EKG changes: Bradycardia, QRS widening, or junctional rhythm are particularly worrisome
Ongoing potassium release: Conditions like tumor lysis syndrome or rhabdomyolysis increase the likelihood of deterioration
Causes
Critically ill patients often develop hyperkalemia due to a combination of several factors such as hypovolemia, renal dysfunction, and the use of medications like ACE inhibitors. Successful treatment may require addressing many of these problems simultaneously
Treatment
- IV calcium to stabilize the myocardium (3g IV calcium gluconate peripherally over 10 minutes or 1g IV calcium chloride centrally over 10 minutes)
- IV insulin plus dextrose to shift potassium into cells (5 units IV insulin and 2 ampules of D50W, adjusted based on blood glucose level)
- Beta-2 agonists such as albuterol (10-20 mg nebulized-->4-8 standard nebs back-to-back)
- IV epinephrine (phenomenal for hyperkalemia-induced bradycardia, because it simultaneously treats both the hyperkalemia and the bradycardia)
- Promote excretion: Using diuretics such as IV furosemide 60-160 mg IV or thiazide (500-1,000 mg IV chlorothiazide, or 5-10 mg metolazone) among patients able to produce urine
- Volume expansion if hypovolemic
- GI binders: Lokelma (10 g TID for 48 hours) or patiromer (8.4 g, repeated daily as needed, less effective than Lokelma)
- Kayexalate is no longer recommended at it has proven to be ineffective and can cause bowel necrosis
- Discontinue any nephrotoxins, establish a state of euvolemia with adequate perfusion, and consider a renal diet with limited potassium intake
- Dialysis: In patients with severe kidney function impairment. Hemodialysis is preferred since the rate of potassium removal is many times faster than with peritoneal dialysis
