History and Physical
- NSAID use? Alcoholism? Liver disease? Surgical hx (gastric bypass, AA)? Prior GI bleeds, colonoscopy, endoscopy? Anticoagulation use, last dose taken?
- POCUS exam: Collapsed IVC indicates volume depletion, ascites easily seen on FAST exam, gastric distension suggests UGI bleed
- Calculate shock index: HR/SBP > 0.9 is a bad sign, frank hypotension
| Upper GI Bleed (75%) (Proximal to Ligament of Treitz) | Lower GI Bleed (Distal to Ligament of Treitz) | |
|---|---|---|
| Symptoms | Hematemesis, Melena, Hematochezia (if bleed is brisk) | Hematochezia |
| Causes | Varices, Cancer, Hemophilia, Arteriovenous malformation (AVM), Gastroesophageal reflux disease (GERD, causing erosive esophagitis), Mallory-Weiss syndrome/Boerhaave syndrome, Peptic ulcer disease (PUD) | Cancer, Hemorrhoids, Ischemia (e.g., colitis, mesenteric ischemia), Diverticulosis, Angiodysplasia, Malignancy |
Testing
- CBC, electrolytes type and screen, coags (INR, PTT, fibrinogen), platelets, LFT's
- BUN/Cr> 36: this means RBC destruction
- >50-60cc blood= melena
- Hyperactive bowel sounds
- Aspirate with NGT (NG lavage)--> more useful in a lower GI bleed to r/o lower bleed
- CT angiography: becoming front-line for lower GI bleeds
AIMS65 Score for Upper GI Bleeding Mortality
Initial Treatment
- 2 large bore IV's (16g)
- IVF (crystalloid)
- NPO
- Transfusion: blood if Hgb < 7 or < 9 in high-risk patients, platelets if plt < 50k, FFP or prothrombin complex for coagulopathy
- Conservative transfusion targets: RCTs and meta-analyses have demonstrated that conservative transfusion causes reduced mortality and reduced rebleeding especially in variceal hemorrhage
- PPI: 40mg IV q12h
- Abx if gastric distension on ultrasound (Erythromycin 250mg IV) prior to intubation/ endoscopy
- If cirrhosis: Octreotide 50mcg bolus then 50mcg/hr infusion and Ceftriaxone 1g
- Discontinue anticoagulants and antihypertensives
Localize the bleed
- Endoscopy (usually first choice as UGI bleeds are more common and often more dangerous)
- Arteriography with IR embolization (for rapid bleeds when acute intervention is required)
- If cause of bleed is not identified: capsule endoscopy (to examine small bowel), tagged RBC scan (for slow, occult bleeds), CT angiography (for faster, active bleeds), push enteroscopy (for small bowel bleeds)
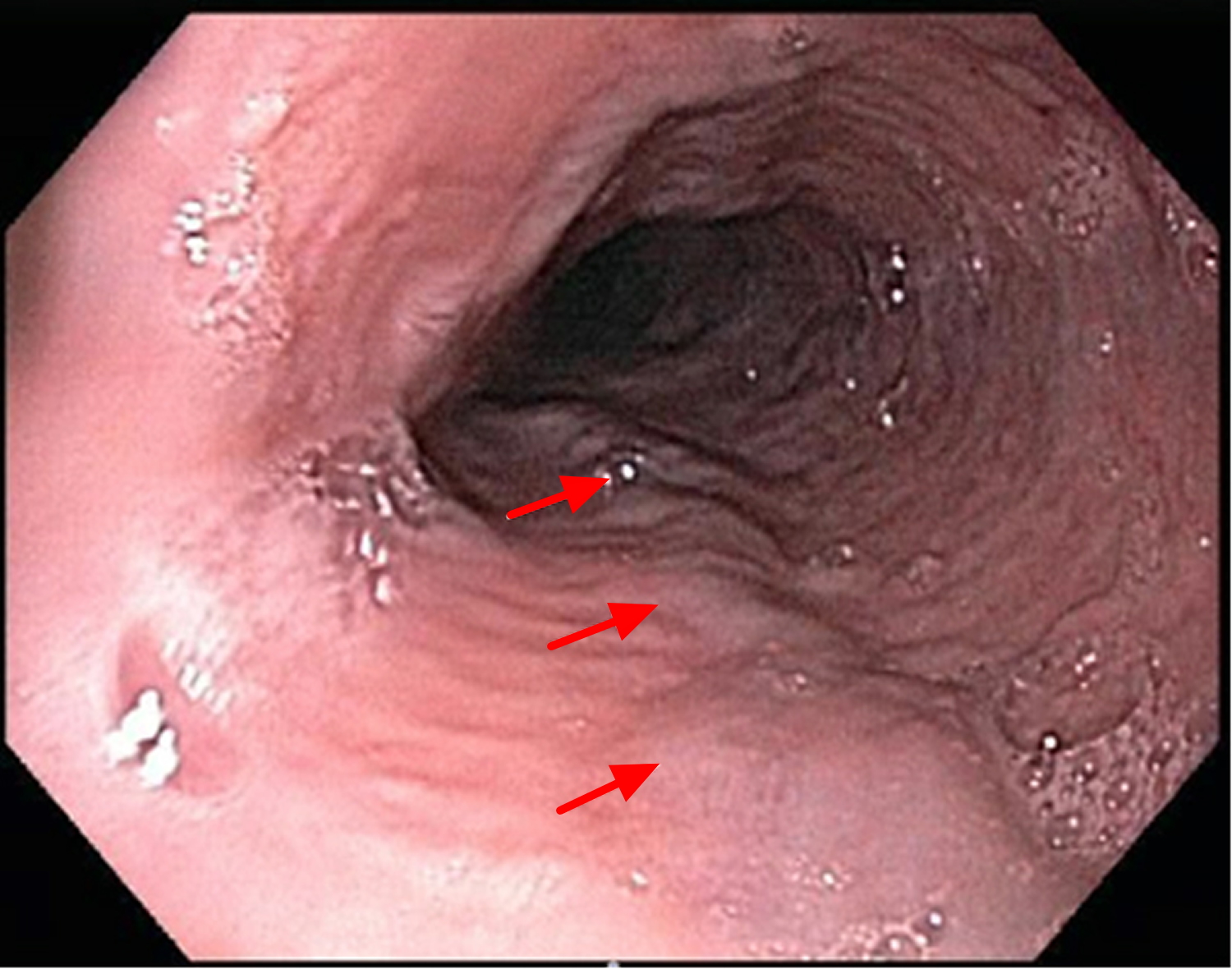
Forrest Classification of Upper GI Bleeding--> Stratifies severity of upper GI bleeding according to endoscopic findings
Forrest Classification Calculator
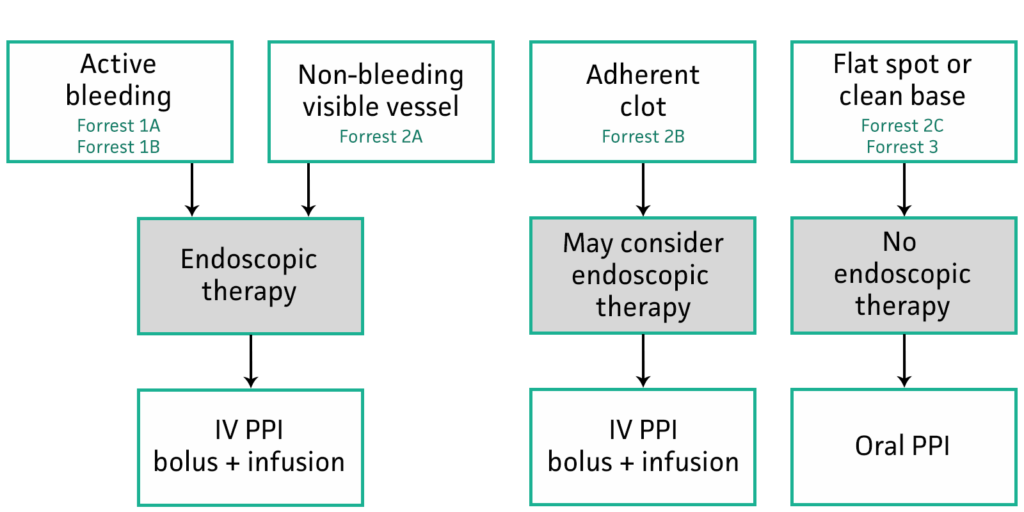
Use Forrest classification to guide decision-making
Stop the bleed
- Esophageal varices: rubber band ligation banding for varices, if this fails then TIPS, Blakemore tube
- Gastric varices: endoscopic therapy, balloon transvenous obliteration, TIPS
- In a brisk LGI bleed, IR is crucial. Too much blood for colonoscopy, IR must embolize
- Epinephrine injection
- Thermocoagulation
- Clipping
