
Definitions
- Chronic bronchitis: Cough > 3 months for at least 2 years
- Emphysema: Enlarged airspaces with alveolar destruction, centrilobular (smokers) vs panlobular (a1 antitrypsin deficiency)
- Asthma-COPD Overlap: Asthma with persistent airflow obstruction
Diagnosis: Original GOLD classification
| Stage | FEV1/FVC Ratio | FEV1 (% predicted) |
|---|---|---|
| GOLD 1 (Mild) | ≥0.70 | ≥80% |
| GOLD 2 (Moderate) | 0.50-0.69 | 50%-79% |
| GOLD 3 (Severe) | 0.30-0.49 | 30%-49% |
| GOLD 4 (Very Severe) | <0.30 | <30% |
Revised GOLD Criteria for Management of COPD
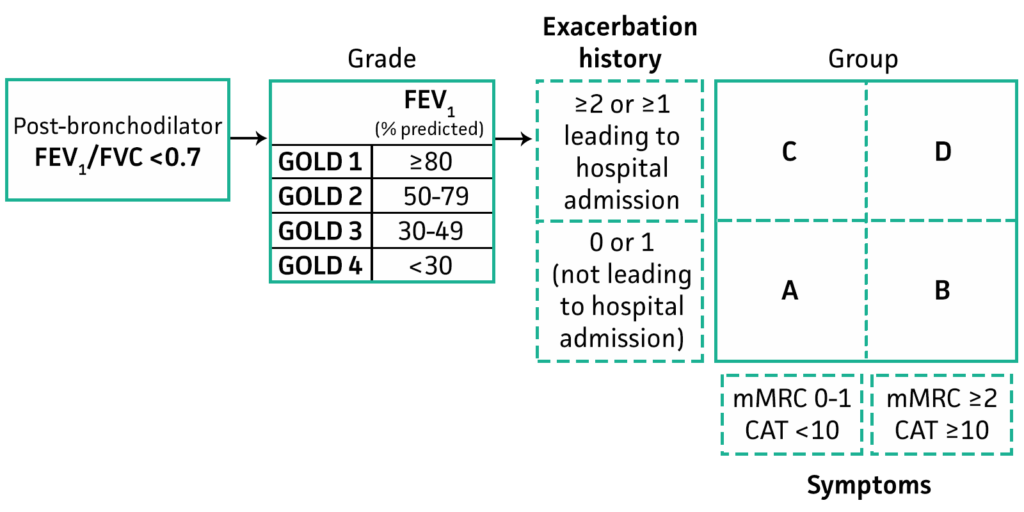
Revised GOLD formula to guide treatment
COPD exacerbation (3 Cardinal Sx)
- Increased cough severity
- Increased sputum production
- Increased dyspnea
Precipitators
Acute Bronchitis/ infection:
- Increased CO2 production, requires increased alveolar ventilation to compensate, but can't fully exhale, so lung volumes and work of breathing increase and more CO2 is produced
- Diaphragmatic fatigue: leads to ↓ TV/RR which ↑ CO2
Diagnostic Workup
- H&P
- Ultrasound
- Chest X-ray
- EKG
- Basic labs (CBC, electrolytes)
- Influenza PCR during flu season
- ABG/VBG generally unhelpful and unnecessary
- Sputum GS/Cx not helpful for AECOPD diagnosis
- Additional options: chest CT scan, procalcitonin (low levels argue against typical bacterial pneumonia)
Differential diagnosis
- Pneumonia: Consolidation on ultrasonography, infiltrate on chest X-ray
- Pulmonary embolism (PE): Lack of usual features of AECOPD (no sputum, no fever, etc.)
- Pulmonary edema: Bilateral B-lines on ultrasonography, signs of congestion on chest X-ray
- Pneumothorax: Loss of lung slide on ultrasonography, pneumothorax on chest X-ray
- Upper airway obstruction: Wheeze/stridor audible without a stethoscope
- Obesity hypoventilation syndrome: Hypercapnic respiratory failure without other COPD findings
- Opioid/sedative effects: Difficulty distinguishing between medication side-effects and underlying COPD-related hypercapnia
Management
Typical regimen for COPD exacerbation: Bronchodilators (ipratroprim and albuterol) + Prednisone 40mg/day for 5 days +- antibiotics
- SABA (albuterol) +/- anticholinergic (ipratroprium)
- Nebulized albuterol/ipratropium q6hr scheduled
- Nebulized albuterol q2hr PRN
- Systemic glucocorticoids--> Start with IV methylprednisolone (e.g., 125 mg IV) & rapidly de-escalate to lower doses (e.g., prednisone 50 mg qd).
- Oxygen goal 88-92%
- NIPPV preferred to mechanical ventilation, HFNC is 2nd line
- Antibiotics indicated if > 2/3 of the main cardinal symptoms
- Uncomplicated COPD (age < 65, FEV1 > 50%, <2 exacerbations/yr): Azithromycin, Doxycycline, TMP-SMX, 2nd/3rd gen cephalosporin
- Complicated COPD (age > 65, FEV1 < 50%, >2 exacerbations/yr): Cover pseudomonas if patient has risk factors (frequent abx use, abx in last 90 days, bronchiectasis, prior pseudomonas ix, FEV1 < 50% predicted)
Monitoring
- BiPAP: Follow tidal volume and minute ventilation
- Respiratory rate: <10 suggests hypoventilation, >30 suggests high work of breathing that may be unsustainable
- pCO2 can rise even in tachypnea, since in COPD pt's can't adequately increase alveolar ventilation, but the patient will excrete the amount of CO2 produced, so each alveoli will need to get rid of more CO2. So CO2 production > CO2 excretion and CO2 rises
PCO2 Calculator → pCO2 = CO2 produced / alveolar ventilation
- Oxygen saturation: Aim for 88-92%
- Mental status/CO2: Follow mental status if patient is arousable and mentating; otherwise, follow ABG/VBG
- pCO2 can actually increase after oxygen therapy due to a paradoxical decrease in respiratory drive and due to Haldane effect (when you give oxygen this displaces CO2 from Hgb), and blood will travel to low V/Q areas, so the less blood to high V/Q areas increases dead space
- Use gestalt (overall clinical impression) as an important factor. Discuss with nurse and respiratory therapist. Follow over time
ABG Targets
- Many COPD patients have chronic hypercapnic respiratory failure, with a chronic compensatory metabolic alkalosis. In this case, ventilation to a normal pCO2 (40mm) is problematic for two reasons:
- Ventilation to a normal pCO2 will cause alkalemia (pH >7.45), which they won't like
- Over time, the kidney will respond to alkalemia by excreting bicarbonate until the serum bicarbonate level is ~24 mEq/L. This will cause problems with trying to get the patient off the ventilator
- The best approach is generally to target a pCO2 close to the patient's baseline value
- In most cases you won't know the patient's baseline. In this situation, targeting a lowish pH (shoot for pH of roughly ~7.25-7.35)
