Definitions
- Heart failure is a complex clinical syndrome with signs and symptoms that result from any structural or functional impairment of ventricular filling or ejection of blood
- Not all leg swelling and shortness of breath is heart failure. Consider a patient’s risk factors and be aware of heart failure mimics
- HFrEF: EF <40%
- HFpEF: EF >50%
- HFmrEF: EF 41-49%
Evaluations of Patients with Heart Failure
Echocardiography in Heart Failure
- Required for patients presenting with signs and symptoms suggestive of heart failure without a previous diagnosis
- Guides initial CHF management by determining appropriate therapies for HFrEF or HFpEF
- Identifies valvulopathy, wall motion abnormalities, and wall thickness that may impact therapy
- Not required in acute decompensation if recent echo available, unless there is a new finding
Ischemic Evaluation
- Consider inpatient ischemic evaluation in high-risk patients
- May be influenced by logistical considerations
- Inpatients with risk factors may undergo ischemic evaluation, but outpatient completion is reasonable in low-risk patients
- Left heart catheterization is not always required; cardiac CTA or stress testing may be an option
POCUS in Heart Failure
- Provides real-time assessment of EF, valvular function, and volume status
- Facilitates early management decisions
Management of Acutely Decompensated Heart Failure
Diuresis
- First-line therapy is decongestion with diuretics
- Monitor electrolytes and renal function to guide dosing decisions
- Vasodilators may help augment diuresis if BP allows
- If hypoperfusion is present, consider escalation of care
- Diuretic-naive: Start with low-dose IV furosemide and reassess in 2 hours
- For patients on chronic diuretics, use the IV equivalent or double the dose
- Consider torsemide or bumetanide for inadequate response to IV furosemide
- Adjunct diuretics may be needed in diuretic resistance
- If inadequate response to bolus therapy, consider continuous infusion
Loop Diuretics and Adjuncts
| Medication | IV Dose | PO Dose | Relative Potency | Benefits |
|---|---|---|---|---|
| Furosemide | 20 mg | 40 mg | 1x | Standard loop diuretic, widely available |
| Torsemide | 10 mg | 20 mg | 2-3x stronger than furosemide | Longer half-life, improved bioavailability |
| Bumetanide | 1 mg | 1 mg | 40x stronger than furosemide | More predictable absorption |
When to Add Adjunct Diuretics
- Metolazone: Often added in diuretic resistance. Common dose: 2.5-5 mg PO daily
- Chlorothiazide: IV option when oral absorption is a concern. Common dose: 250-500 mg IV daily
- Consider adjuncts when urine output remains inadequate despite high-dose loop diuretics
- Sequential nephron blockade with thiazides can enhance diuresis
- SGLT2 inhibitors also have diuretic effects and should be considered early if renal function allows
Monitoring Diuretic Response
- Accurate I/Os and daily weights are essential
- Be mindful of malnutrition in prolonged hospitalizations
- Consider fluid restriction in cases of severe hyponatremia
- Avoid strict sodium restriction beyond a general 2g/day limit
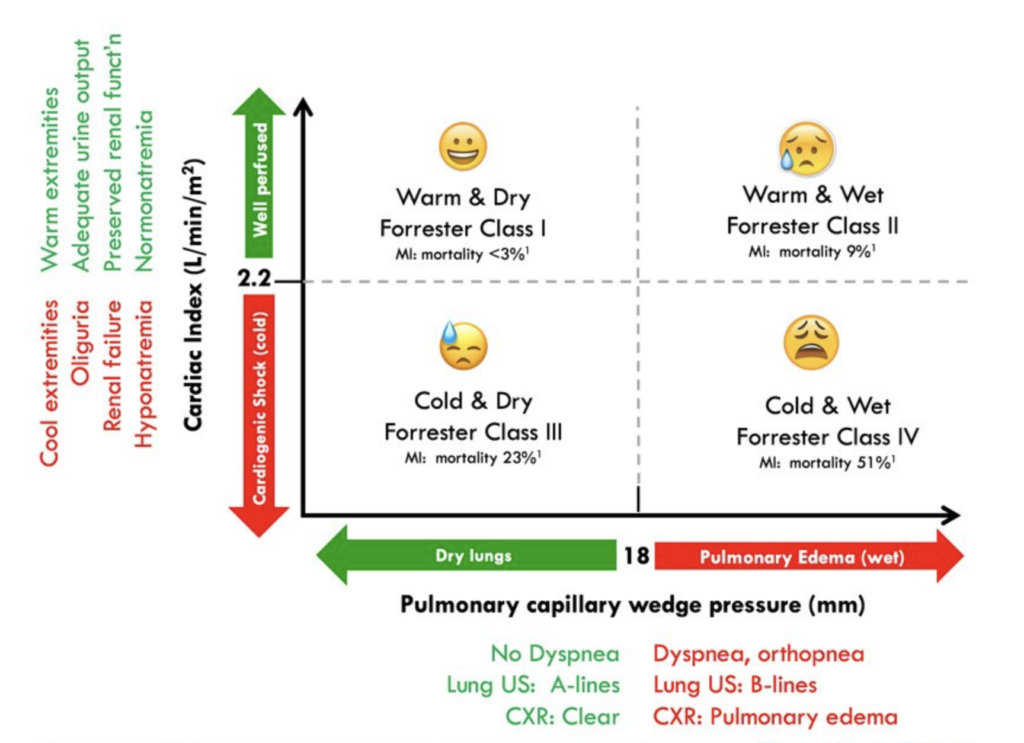
The Decompensating Heart Failure Patient
- Stop BP-lowering medications in cardiogenic shock
- Escalate care rapidly and utilize institutional resources for shock management
- No clear data favoring one vasopressor over another
- Norepinephrine is preferred in severe hypotension
- Consider milrinone or dobutamine for inotropic support
- If non-responsive to therapy, consider right heart catheterization
| Parameter | Milrinone | Dobutamine |
|---|---|---|
| Dose | 0.125-0.75 mcg/kg/min (no loading dose in acute decompensation) | 2-20 mcg/kg/min |
| Mechanism of Action | PDE-3 inhibitor, increases cAMP leading to vasodilation and inotropy | Beta-1 agonist, increases heart rate and contractility |
| Hemodynamic Effects | Increased cardiac output, reduced SVR and PVR, mild chronotropic effect | Increased cardiac output, mild vasodilation, more pronounced chronotropic effect |
| Efficacy | Useful in cardiogenic shock, especially with concomitant pulmonary hypertension or RV dysfunction | Preferred in cardiogenic shock with low cardiac output and hypotension |
| Side Effects | Hypotension (due to vasodilation), arrhythmias, thrombocytopenia | Tachycardia, arrhythmias, increased myocardial oxygen demand |
| Renal Considerations | Excreted renally, prolonged half-life in renal dysfunction | No renal dose adjustment needed |
| Indications | Cardiogenic shock with high SVR and preserved BP, pulmonary hypertension, RV failure | Cardiogenic shock with low BP, acute decompensated heart failure with hypotension |
| Best Situations | When afterload reduction is beneficial, patients with pulmonary hypertension or RV dysfunction | When BP support is needed alongside inotropy |
GDMT
Therapies for HFrEF
- Four pillars: Beta blockers, SGLT2 inhibitors, ARB/ARNIs, aldosterone antagonists
- Sequence varies based on BP, renal function, and hospitalization course
- SGLT2 inhibitors should be introduced early for diuresis benefits
- Aldosterone antagonists can be initiated if hypokalemia occurs
- Beta blockers should not be started on the day of discharge; initiate at least 24 hours before discharge
- ARNIs should be introduced after adequate decongestion due to hypotension risk
Therapies for HFpEF
- SGLT2 inhibitors benefit all genders and EF ranges
- ARNIs may be more beneficial in men with EF <60%
- Aldosterone antagonists reduce hospitalizations and improve diuresis
- Beta blockers are not indicated unless required for arrhythmia or CAD
Preparing for Discharge
- Literature supports rapid up-titration of GDMT
- Prioritize starting low doses of all four GDMT pillars rather than maximizing single therapies
- Follow-up should occur within one week
- Patient education on medications, side effects, and follow-up is crucial
