Definitions
| Type of Heart Failure | Ejection Fraction (EF) | Characteristics and Causes |
|---|---|---|
| Heart Failure with Reduced EF (HFrEF) | EF < 40% | Weakened heart muscle; reduced ability to contract and pump |
| --> Associated with coronary artery disease, heart attacks, etc. | ||
| Heart Failure with Preserved EF (HFpEF) | EF > 50% | Stiff heart muscle; impaired relaxation and filling |
| --> Linked to hypertension, aging, obesity, and valve disorders | ||
| Heart Failure with Mid-Range EF (HFmrEF) | 40% ≤ EF ≤ 50% | Intermediate category, shares characteristics of HFrEF and HFpEF |
| --> Treatment approach may involve aspects of both types |
- Clinically you cannot differentiate HFrEF from HFpEF, so you need an echocardiogram
- One exception is only HFrEF causes low output symptoms like hypotension, cool extremities, and cachexia
- BNP levels can be normal inHFpEF: At rest their filling pressures may not be elevated, but when exercise both tachycardia (due to decreased RR interval) and hypertension decrease lusitropy, resulting in increased filling pressures and BNP levels
- BNP levels can be elevated in atrial fibrillation, chronic kidney and pulmonary disease even if not in heart failure
Clinical Manifestations
| NYHA Class | Description |
|---|---|
| Class I | No limitation of physical activity. Ordinary physical activity does not cause undue fatigue, palpitation, or dyspnea (shortness of breath). |
| Class II | Slight limitation of physical activity. Comfortable at rest, but ordinary physical activity results in fatigue, palpitation, or dyspnea. |
| Class III | Marked limitation of physical activity. Comfortable at rest, but less than ordinary activity causes fatigue, palpitation, or dyspnea. |
| Class IV | Unable to carry out any physical activity without discomfort. Symptoms of heart failure at rest. If any physical activity is undertaken, discomfort increases. |
- Gradual onset with progressive fluid retention and systemic congestion
- Symptoms include progressive dyspnea, abdominal and peripheral congestion, nocturia, and neurologic symptoms
- Physical signs show signs of congestion, elevated jugular venous pressure, tender/enlarged liver, pleural effusion, rales, and leg edema
ADHF with Severe Pulmonary Edema
- Seen in <3% of ADHF patients
- Rapid onset with predominant pulmonary congestion
- Symptoms include suffocation, anxiety, cough, pink frothy expectoration, and sensation of drowning
- Physical signs include increased respiratory rate, dilated alae nasi, inspiratory retractions, elevated pulse rate, and coarse lung sounds
Cardiogenic Shock
- Present in 3.6% of acutely decompensated HF patients
- Low-output HF with decreased end-organ perfusion
- Symptoms include fatigue, altered mental status, and signs of organ hypoperfusion
- Physical signs may show tachypnea, tachycardia, cold/cyanotic periphery, diminished pulse pressure, and pulsus alternans
High-Output Heart Failure
- Uncommon cause of ADHF
- Presents with warm extremities, pulmonary congestion, tachycardia, and wide pulse pressure
- Underlying causes include anemia, obesity, thyrotoxicosis, liver failure, and skeletal conditions.
Right-Sided Heart Failure
- Common in severe tricuspid regurgitation, right ventricular dysfunction, and chronic lung disease
- Presents with signs of right-sided volume overload
- Pulmonary embolism as a cause of dyspnea and right HF should be excluded
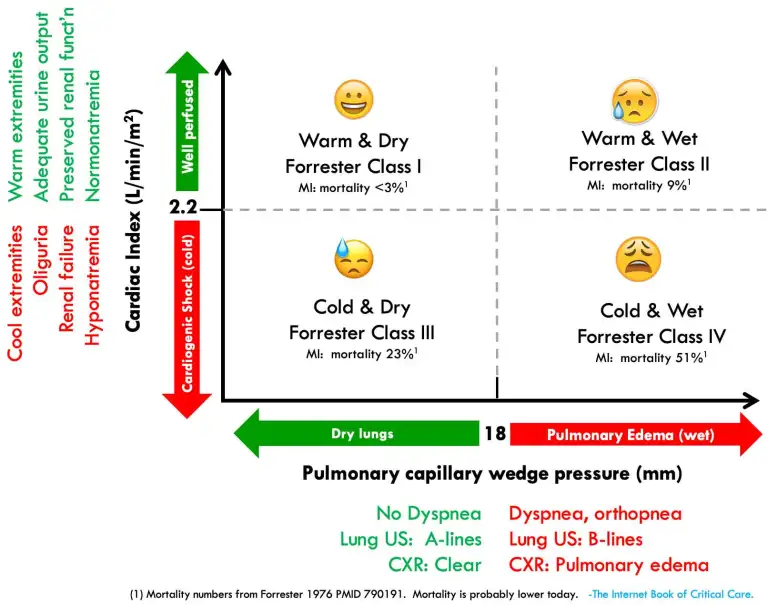
Forrester classification of heart failure based on cardiac index (systemic perfusion) and pulmonary capillary wedge pressure (pulmonary congestion)
Workup
Initial testing for patients with acute decompensated heart failure (ADHF) includes a 12-lead ECG, chest radiograph, and laboratory tests
- The 12-lead ECG assesses for evidence of acute coronary syndrome (ACS) and arrhythmias
- Chest radiograph helps evaluate pulmonary congestion, cardiomegaly, and pleural effusions
- Lung ultrasound (LUS) can be used as an adjunctive diagnostic modality, especially for assessing pulmonary edema
Laboratory tests include pulse oximetry, ABG, routine chemistries, lactic acid level (in shock or marked weakness), troponin levels (for possible ACS), CBC, and natriuretic peptide levels (BNP or NT-proBNP)
Echocardiography: Recommended for patients with new HF, suspected change in cardiac function, or valvular heart disease
HFreF vs. HFpEF Causes and Triggers
Etiologies of Heart Failure
| Depressed Ejection Fraction (<40%) | Preserved Ejection Fraction (>50%) | |
|---|---|---|
| Common Causes | Coronary artery disease, Myocardial infarction, Chronic ischemia, Chronic pressure/volume overload (such as mitral regurgitation), Hypertension, Obstructive valvular disease, tachycardia (from Afib) | Hypertension, Pathologic hypertrophy (Primary or Secondary), Aging, Endomyocardial disorders, Chronic kidney disease, Diabetes |
| Less Common Causes | Nonischemic dilated cardiomyopathy, Familial/genetic disorders, Infiltrative disorders, Toxic/drug-induced damage, Viral, Alcohol, Cancer chemotherapy, Disorders of rate and rhythm | Restrictive cardiomyopathy, Infiltrative disorders (like Transthyretin amyloidosis and sarcoidosis), Storage diseases (like hemochromatosis), Fibrosis, Chronic ischemia |
Precipitators of Heart Failure
| Depressed Ejection Fraction (<40%) | Preserved Ejection Fraction (>50%) | |
|---|---|---|
| Common Precipitators | Medication noncompliance, Increased dietary sodium intake, Decline in renal function, Hypertension, Certain medications that decrease contractility or increase afterload, NSAIDs, | Medication noncompliance, Increased dietary sodium intake, Decline in renal function, Hypertension, Certain conditions requiring increased cardiac output, Brady-arrhythmia, Tachyarrhythmia |
| Specific Medications to Consider | Non-dihydropyridine and dihydropyridine (except amlodipine) calcium channel blockers; some anti-arrhythmics like flecanide, soltalol, and propafenone; ACE inhibitors, ARBs, beta blockers | Certain diabetic medications like pioglitazone; potentially beneficial medications like GLP-1 and SGLT2 inhibitors |
- Hypertension causes ↓ lusitropy in HFpEF & ↓ stroke volume in HFrEF
- In HFrEF avoid medications that ↓ contractility (verapamil/diltiazem) and medications that ↑ afterload (ACEIs)
- Never begin beta blockers during acute exacerbation, but once on them don't stop unless cardiogenic shock/ hypotension/ bradycardia
- NSAIDs cause sodium retention, decrease renal function, increase blood pressure by preventing vasodilation by prostaglandins
- In both HFrEF and HFpEF a condition that require an increase in cardiac output (infections) can precipitate heart failure due to need to ↑ stroke volume which ↑ LVEDP
- Afib with RVR: short R-R intervals will cause ↓ lusitropy, due to less time to fill during diastole resulting in ↑ LVEDP, but also decreased filling due to losing atrial kick (which they depend on), so following beat has ↓ EF
- Iatrogenic fluid overload: ED loves bolusing everyone with a couple liters of NS with an infection. If patient has CHF w/ infection capillaries are leaky and fluids increase preload, but CHF patients (diastolic dysfunction) don't allow increasing cardiac output so they develop pulmonary edema
HFrEF Treatment
| Therapies/Interventions | Description |
|---|---|
| Oxygen and Noninvasive Positive Pressure Ventilation (NIPPV) | Used for respiratory support |
| Medical Therapy | Includes vasodilators, diuretics, inhibition of neurohormonal activation |
| Inotropic Therapies/Mechanical Circulatory Support | Used for organ hypoperfusion |
| Arrhythmia Management | Pharmacologic rate control or cardioversion may be considered |
| Clevidipine | Can be effective for reducing blood pressure and improving dyspnea |
| Diuretics | Cornerstone of therapy for acute heart failure. Loop diuretics preferred initially (IV administration). Transition to oral diuretic therapy when near-euvolemic state is reached |
| Vasodilators | Includes nitroprusside, nitrates, nesiritide. Used for symptom relief. Nitrates decrease preload and relieve dyspnea. Sodium nitroprusside used for severe pulmonary congestion. Nesiritide reduces pulmonary pressures but does not affect heart contractility |
| Ultrafiltration | Effective alternative to IV diuretics in some cases. Removes fluid without significant changes in electrolyte concentration |
| Hospitalization Indications | Severe acute decompensated heart failure, dyspnea at rest, hemodynamically significant arrhythmia, acute coronary syndrome, worsening congestion, electrolyte abnormalities, comorbid conditions, etc. |
| Invasive Hemodynamic Monitoring | Not indicated for stable patients responding to medical therapy. Indicated in cases of respiratory distress, impaired perfusion, etc. |
| Discharge Criteria | Stable oral regimen for at least 24 hours, addressed exacerbating factors, optimized volume status, transitioned to oral diuretic therapy, stable clinical status, patient and family education, post-discharge instructions, follow-up arrangements |
| ARNI Use | Considered in recently hospitalized stable patients with heart failure with reduced ejection fraction (HFrEF), even if ACEI/ARB not previously given |
| Afterload reduction | Particularly helpful in mitral regurgitation and aortic regurgitation since they are volume dependent |
GDMT for HFrEF
| Medication | Starting Dose | Target Dose |
|---|---|---|
| Beta-Blockers: improve heart failure outcomes by reducing heart rate, improving diastolic filling time, and decreasing myocardial oxygen demand. They also promote reverse remodeling of the heart, leading to improved cardiac function and decreased symptoms | ||
| - Bisoprolol | 1.25 mg once daily | 10 mg once daily |
| - Carvedilol | 3.125 mg twice daily | 25 mg (weight <85 kg) or 50 mg (weight ≥85 kg) twice daily |
| - Metoprolol succinate | 12.5–25 mg daily | 200 mg daily |
| ARNIs: combine an angiotensin receptor blocker (ARB) with a neprilysin inhibitor. The ARB blocks the action of angiotensin II, a hormone that causes blood vessel constriction and fluid retention. The neprilysin inhibitor increases the levels of beneficial peptides that promote vasodilation and sodium excretion. combine an angiotensin receptor blocker (ARB) with a neprilysin inhibitor. The ARB blocks the action of angiotensin II, a hormone that causes blood vessel constriction and fluid retention. The neprilysin inhibitor increases the levels of beneficial peptides that promote vasodilation and sodium excretion | ||
| - Sacubitril/valsartan | 24/26 mg–49/51 mg twice daily | 97/103 mg twice daily |
| ACEIs: combine an angiotensin receptor blocker (ARB) with a neprilysin inhibitor. The ARB blocks the action of angiotensin II, a hormone that causes blood vessel constriction and fluid retention. The neprilysin inhibitor increases the levels of beneficial peptides that promote vasodilation and sodium excretion | ||
| - Captopril | 6.25 mg 3× daily | 50 mg 3× daily |
| - Enalapril | 2.5 mg twice daily | 10–20 mg twice daily |
| - Lisinopril | 2.5–5 mg daily | 20–40 mg daily |
| - Ramipril | 1.25 mg daily | 10 mg daily |
| ARBs: ARBs block the action of angiotensin II by binding to its receptors, preventing its vasoconstrictive and fluid-retaining effects. Effect on Heart Failure: ARBs have similar effects to ACEIs in improving heart failure outcomes. They reduce blood vessel constriction, decrease fluid retention, improve cardiac function, and promote reverse remodeling of the heart. | ||
| - Candesartan | 4–8 mg daily | 32 mg daily |
| - Losartan | 25–50 mg daily | 150 mg daily |
| - Valsartan | 40 mg twice daily | 160 mg twice daily |
| Aldosterone antagonists: Aldosterone antagonists block the action of aldosterone, a hormone that promotes sodium and water retention in the kidneys. Effect on Heart Failure: Aldosterone antagonists improve heart failure outcomes by reducing fluid retention and preventing adverse cardiac remodeling. They also have anti-inflammatory and anti-fibrotic effects, leading to improved cardiac function and decreased mortality rates. | ||
| - Eplerenone | 25 mg daily | 50 mg daily |
| - Spironolactone | 12.5–25 mg daily | 25–50 mg daily |
| SGLT2 inhibitors: SGLT2 inhibitors block the SGLT2 protein in the kidneys, reducing glucose reabsorption and increasing glucose excretion in the urine. They also lead to a mild diuretic effect and promote ketone body utilization. Effect on Heart Failure: SGLT2 inhibitors have been shown to improve heart failure outcomes by reducing heart failure hospitalizations, cardiovascular events, and mortality rates. They also have cardioprotective effects, including reducing oxidative stress, inflammation, and myocardial fibrosis. | ||
| - Dapagliflozin | 10 mg daily | 10 mg daily |
| - Empagliflozin | 10 mg daily | 10 mg daily |
| Vasodilators: SGLT2 inhibitors block the SGLT2 protein in the kidneys, reducing glucose reabsorption and increasing glucose excretion in the urine. They also lead to a mild diuretic effect and promote ketone body utilization. Effect on Heart Failure: SGLT2 inhibitors have been shown to improve heart failure outcomes by reducing heart failure hospitalizations, cardiovascular events, and mortality rates. They also have cardioprotective effects, including reducing oxidative stress, inflammation, and myocardial fibrosis. | ||
| - Hydralazine | 25 mg 3× daily | 75 mg 3× daily |
| - Isosorbide dinitrate | 20 mg 3× daily | 40 mg 3× daily |
| - Fixed-dose combination isosorbide dinitrate/hydralazine | 20 mg/37.5 mg (1 tab) 3× daily | 2 tabs 3× daily |
| - Ivabradine | 2.5–5 mg twice daily | Titrate to heart rate 50–60 beats/min. Maximum dose 7.5 mg twice daily |
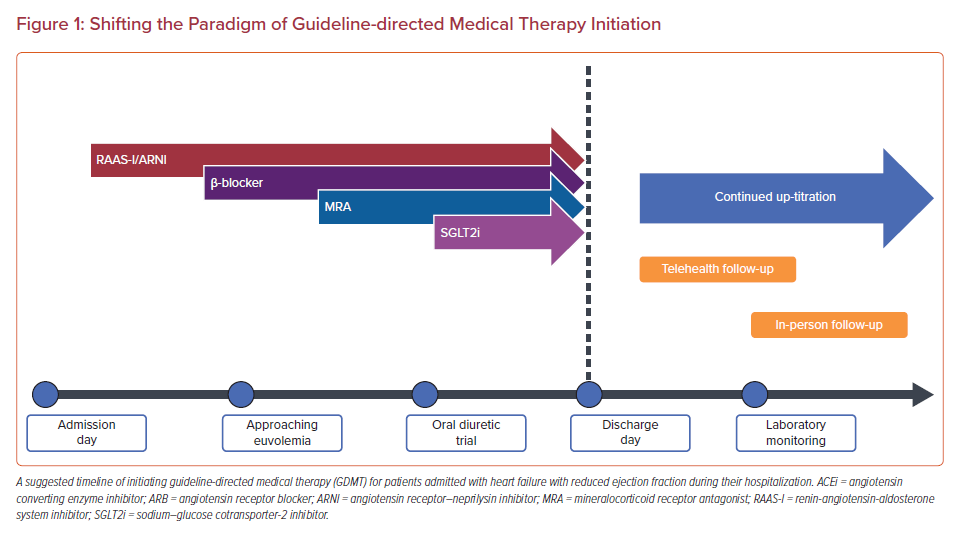
Inpatient GDMT management
HFpEF Management
- Loop diuretics
- Suggest treatment with both a sodium-glucose co-transporter 2 (SGLT2) inhibitor and a mineralocorticoid receptor antagonist (MRA)--> start the SGLT2 inhibitor first and then add the MRA two weeks later if the patient tolerates initial therapy
- For patients with HFpEF who have poorly controlled hypertension and persistent HF symptoms despite optimal SGLT2 inhibitor and MRA therapy--> add Entresto
When to discontinue ACE inhibitor during CHF exacerbation/ AKI?
- ACEIs dilate the efferent arteriole and thus ↓ GFR
- But they decrease mortality in CHF and improve cardiac output
- 10-15% drop in GFR is normal
- If hyperkalemia occurs, add a potassium binder (Lokelma/Patiromer) or SGLT2 inhibitor to excrete more K+
- ACE inhibitor therapy should not be discontinued unless serum creatinine level rise above 30% over baseline during the first 2 months after initiation of therapy
Cardiogenic Shock
In case of severe heart failure or suspected cardiogenic shock, evaluate with EKG and echocardiography, and conduct lab tests such as Troponin, Lactate, and liver function. Consider testing for TSH and/or digoxin level based on context.
Treatment Approaches
- Lungs: In cardiogenic pulmonary edema, consider BiPAP or intubation. Drain any large effusions causing acute distress. Inhaled epoprostenol might be used for intubated patients with right ventricular failure or pulmonary hypertension.
- Mean Arterial Pressure (MAP) Optimization: For hypertension or normotension, use afterload reduction strategies such as Nitroglycerine infusion or a combination of hydralazine and isosorbide dinitrate. For severe hypotension with organ dysfunction, consider using Norepinephrine, or Epinephrine in HFrEF with hypoperfusion.
- Volume Optimization: Perform a fluid challenge in case of hypoperfusion, absence of pulmonary congestion, and if assessment suggests total body hypovolemia. Consider diuresis for significant systemic/pulmonary congestion and total body volume overload.
- Dobutamine Consideration: In HFrEF, consider using dobutamine in a normotensive patient with organ hypoperfusion or in a hypotensive patient with refractory cardiogenic pulmonary edema. Digoxin may be considered as a weak inotropic agent in patients with chronic AF, HFrEF, and refractory heart failure.
- Underlying Etiology Treatment: Treat new-onset tachyarrhythmia causing heart failure with cardioversion and antiarrhythmics. Treat bradycardia or an inappropriately slow heart rate. For ischemic cardiomyopathy, consider revascularization and treatment for acute MI if present.
- Mechanical Circulatory Support: Consider this for persistent organ failure. The choice of device is patient and institution specific.
- Things to Avoid: Avoid nephrotoxins like NSAIDs, ACE-inhibitors, and angiotensin receptor blockers. Do not initiate a beta-blocker in decompensated heart failure. Avoid any beta-blocker or calcium-channel blocker (like diltiazem) in a patient with cardiogenic shock.