To culture or not to culture?
Clinical Scenarios
The article presents two clinical cases in which the necessity of blood cultures for diagnosing bacteremia is discussed. The first case is a 62-year-old woman with worsening cough, shortness of breath, and fever, but without leukocytosis. The second case is a 47-year-old man with postoperative fever and leukocytosis, with clinical suspicion of septic arthritis.
Context
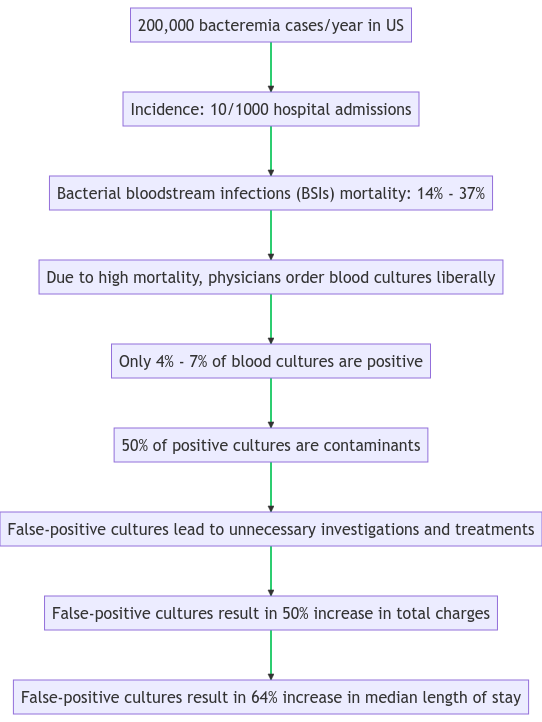
Blood cultures are often liberally ordered in patients suspected of bacteremia, although only a small proportion yield true-positive results. The authors aim to assess the accuracy of clinical and laboratory findings in the decision to obtain blood cultures for suspected bacteremia.
Importance
Approximately 200,000 episodes of bacteremia occur in the United States each year. It is associated with a mortality rate of 14%-37%. Because of the high mortality associated with bacteremia, physicians tend to order blood cultures liberally, resulting in only 4%-7% positive blood cultures.
Examination for Bacteremia
Examine the patient's history, vital signs, cardiovascular, pulmonary, abdominal, and mental status. Additionally, laboratory evaluations like a complete blood count, assessment of base deficit and elevated serum lactate levels, and evaluation of acute kidney injury should be conducted.
Data Sources and Study Selection
35 studies were selected from MEDLINE and EMBASE, representing 4566 bacteremia and 25,946 negative blood culture episodes.
Data synthesis
The study reveals that the pretest probability of bacteremia varies depending on the clinical context. Elevated temperatures and isolated leukocytosis are not accurate predictors of bacteremia. The severity of chills and the presence of systemic inflammatory response syndrome (SIRS) and a multivariable decision rule with major and minor criteria are sensitive predictors of bacteremia.
Results
- The study found that clinical variables like fever, chills, and certain physical and historical clues can help predict bacteremia. The study stresses the importance of interpreting these findings in context with the patient's pretest probability of bacteremia.
- Few historical features are assessed in multiple studies. Prior antibiotic use gives a likelihood ratio (LR) of 0.63 (95% CI, 0.41-0.98), suggesting a slightly decreased likelihood of bacteremia. However, the studies do not clarify whether these data may represent false-negative blood culture results
- Regarding physical examination, tachycardia alone (heart rate >100/min) was not a significant predictor of bacteremia. Presence of hypotension or shock almost doubled the likelihood of bacteremia
- White blood cell (WBC) counts and cellular differential are the most widely used laboratory tests. WBC thresholds from 10,000 to 15,000/L did not produce an LR higher than 1.7. The presence of increased immature (band) forms of neutrophils gave similar information to total WBC counts. Thrombocytopenia increased the likelihood of bacteremia, with a positive LR of 2.0-2.1. Lymphopenia (lymphocyte count <500/L or 1000/L) and a neutrophil-lymphocyte ratio greater than 10 were associated with bacteremia.
Clinical Impression
Pfitzenmeyer et al found that a clinician's impression of the likelihood of bacteremia can be useful. High perceived probability increased the likelihood of bacteremia, with an LR of 2.3 (95% CI, 1.4-3.6), while low perceived probability decreased it.
Individual symptoms and signs do not significantly alter the likelihood of bacteremia. Hence, the research looked at combinations of findings. Systemic Inflammatory Response Syndrome (SIRS) and a clinical decision rule developed by Shapiro et al were used. SIRS increased the likelihood of bacteremia, with a positive LR of 1.8 (95% CI, 1.6-2.0), while its absence significantly decreased the likelihood.
Limitations
The study acknowledges limitations, including that the probability of bacteremia in the studies was generally higher than for series of consecutive blood cultures. This discrepancy is likely due to patient selection based on signs or symptoms suggestive of bacteremia, possibly resulting in biased estimates of the LRs. There were no studies of large numbers of patients with common immunocompromising conditions such as HIV/AIDS, malignancy, or immunosuppressive drug use.
Case Scenario Conclusions
Case 1 represents a situation where blood cultures should not be ordered, given the patient's low probability of bacteremia
For Case 2, the likelihood of bacteremia is substantial due to the presence of tachycardia, knee effusion and pain, and elevated creatinine level, suggesting a possible postoperative infection. As such, ordering blood cultures would be a justified course of action.
Take Home Message
Blood cultures should not be ordered for adult patients with isolated fever or leukocytosis without considering the pretest probability. SIRS and the decision rule may be helpful in identifying patients who do not need blood cultures.
Coburn B, Morris AM, Tomlinson G, Detsky AS. Does This Adult Patient With Suspected Bacteremia Require Blood Cultures? JAMA. 2012;308(5):502–511. doi:10.1001/jama.2012.8262
