Pearls
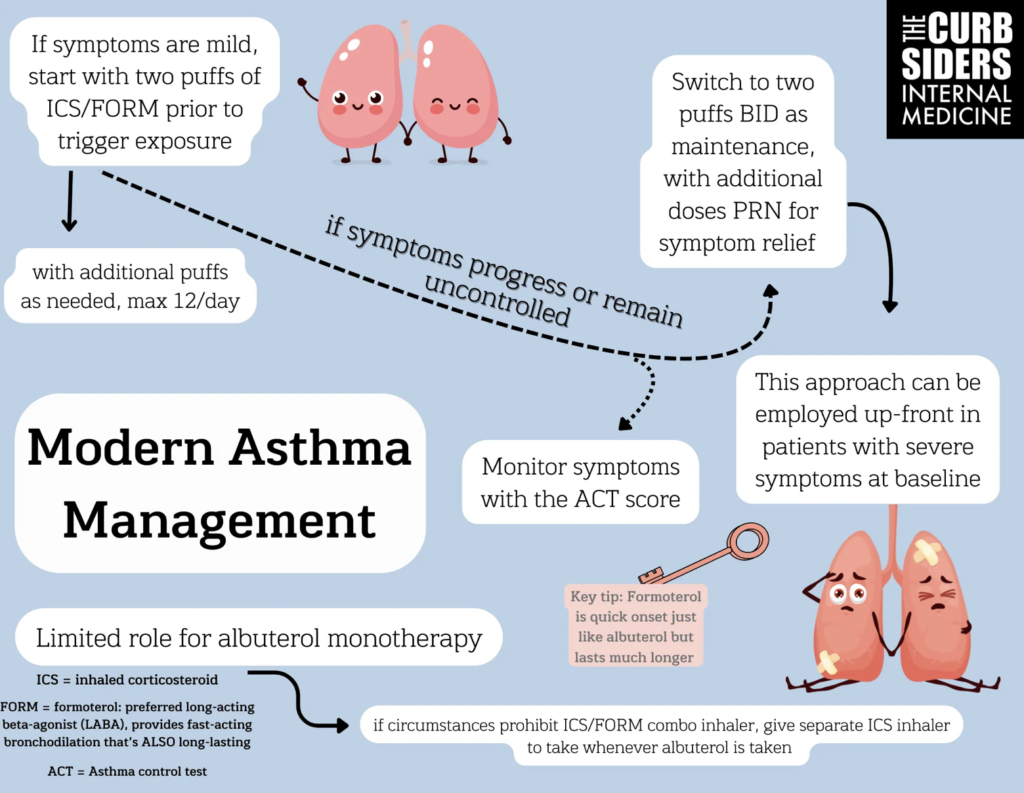
- Avoid SABA monotherapy; prioritize ICS-formoterol as the new reliever therapy given the fast onset of formoterol. It can be used as a maintenance inhaler if more control is needed. Avoid salmeterol due to delayed onset.
- For patients with a SABA who are unable to obtain access to ICS-formoterol, tell them to use an ICS inhaler whenever they use their SABA.
- Clinical history is important. In addition to assessing asthma triggers like dust, wildfires, and pollen, ask about a history of premature birth (before 34 weeks) as this increases the risk of bronchopulmonary dysplasia and underdeveloped terminal airways, which is a risk factor for asthma.
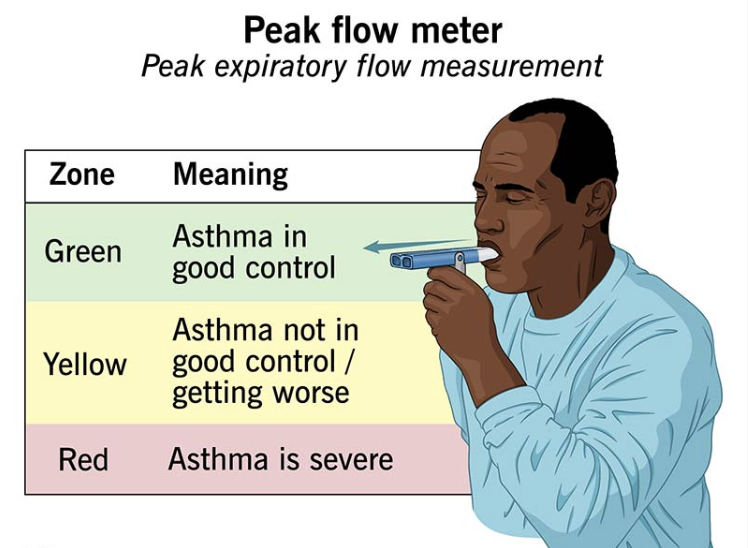
- Spirometry should be used to diagnose asthma, but peak expiratory flow (PEF) can be used if spirometry is unavailable.
- When spirometry is normal during asymptomatic periods, use bronchoprovocation testing with methacholine to confirm airway hyperresponsiveness. This is particularly sensitive for diagnosing asthma.
- Utilize the ACT questionnaire to assess and monitor asthma control over time. Scores below 20 suggest poorly-controlled asthma and should prompt therapy adjustments.
- Refer early for severe or poorly-controlled asthma, asthma-COPD overlap, or obesity-associated asthma.
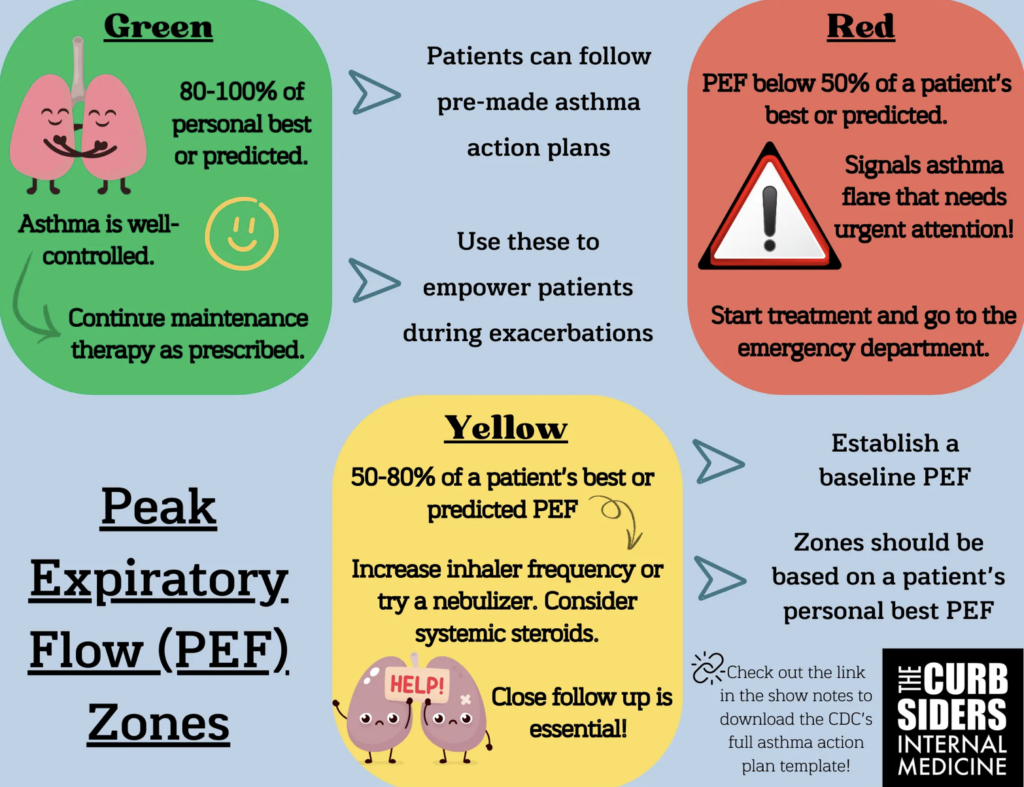
- Use personal PEF measurements to assist in creating an asthma action plan, which can aid in diagnosing and triaging asthma exacerbations.
- Encourage healthy weight management, regular exercise, routine vaccination, and pulmonary rehabilitation to improve asthma outcomes.
Conducting the Initial Interview
Patient History
- Start with an open-ended question, then assess specific triggers
- Environmental factors: dust, pollen, air quality, wildfires
- Physical activity as a trigger
- Family history of asthma or lung disease
- Childhood history: premature birth (before 34 weeks) linked to bronchopulmonary dysplasia
- Ask about childhood asthma and why symptoms may improve with age
Making the Diagnosis of Asthma
Gold Standard: Spirometry
- Obstructive airway disease with reversibility after bronchodilator
- FEV1/FVC reduction alone is not enough for diagnosis
- FEF 25-75% can indicate early-stage obstruction
PFT Findings in Asthma
| Test | Findings in Asthma | Notes |
|---|---|---|
| FEV1/FVC Ratio | ↓ (Reduced) (<0.75-0.80) | Hallmark of obstructive lung disease |
| FEV1 (Post-Bronchodilator) | ↑ by ≥12% and ≥200 mL improvement | Confirms reversible airway obstruction |
| FEF 25-75% | ↓ (Reduced) | Suggests early small airway involvement |
| TLC (Total Lung Capacity) | Normal or ↑ | Hyperinflation may occur in severe cases |
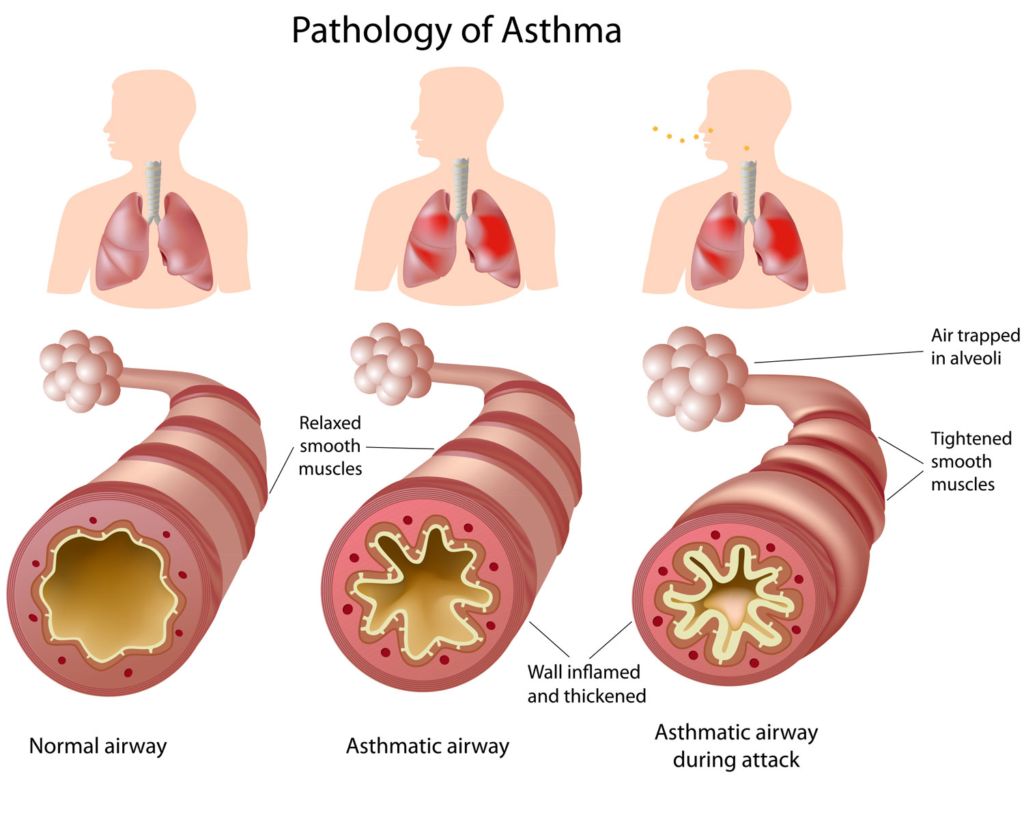
| RV (Residual Volume) | ↑ (Increased) | Air trapping due to airway obstruction |
| DLCO (Diffusion Capacity) | Normal | Differentiates from COPD (which may have ↓ DLCO) |
| Methacholine Challenge | FEV1 ↓ by ≥20% at low doses | Indicates airway hyperreactivity when spirometry is normal |
Key Takeaway:
- Reversible obstruction is the hallmark of asthma
- Methacholine challenge is useful when spirometry is normal but asthma is suspected
Bronchoprovocation Testing
- Needed if spirometry is normal during asymptomatic periods
- Methacholine challenge to assess hyperreactivity
- Exercise test for exercise-induced bronchoconstriction
Considerations for Pregnant Patients
- Spirometry may be confounded but can still be attempted
- Asthma control changes: one-third improve, one-third worsen, one-third remain stable
Is Spirometry Always Necessary?
- Essential for diagnosis but can be skipped in select cases
- Empiric ICS-formoterol trial may be reasonable if spirometry is unavailable
Peak Expiratory Flow (PEF) Testing
- Best for monitoring asthma over time
- Can be used for diagnosis in resource-limited settings
- Assess >10% variability over two weeks
- Bronchodilator response: >20% increase suggests asthma
Staging Asthma
- Symptoms only in specific circumstances
- Mild but persistent symptoms
- Severe symptoms interfering with daily life
The Asthma Control Test (ACT)
- Validated questionnaire for symptom control
- Five questions assessing symptoms, inhaler use, and perception of control
- Score ≥20 = well-controlled, ≤19 = not well-controlled
Asthma Control Test™
Know your score
The Asthma Control Test™ provides a numerical score to help you and your healthcare provider determine if your asthma symptoms are well controlled.
Asthma Management
Formoterol + ICS (Symbicort) as the New Albuterol
- Superior to albuterol monotherapy
- If mild symptoms -> 2 puffs Symbicort prior to trigger exposure with additional puffs as needed (max 12/day)
- If symptoms worsen/poorly controlled -> 2 puffs Symbicort BID as maintenance with additional doses PRN for symptom relief
- Addresses airway inflammation while providing symptom relief
- Reduces exacerbations and systemic steroid use
- Formoterol preferred over salmeterol due to rapid onset (5-10 min vs 2 hours)
- Albuterol-ICS may be an alternative for patients reluctant to switch to formoterol
Practical Application
- PRN ICS-formoterol for mild asthma
- Maintenance And Reliever Therapy (MART) for worsening symptoms
- High-dose therapy for frequent exacerbations, step down once controlled
Cost-Conscious Options
- If ICS-formoterol is too expensive, use separate ICS and bronchodilator inhalers
Montelukast
- Adjunct for allergic, exercise-induced, or aspirin-sensitive asthma
- Risk of neuropsychiatric side effects (black box warning)
- Not used as monotherapy except possibly for cough-variant asthma
Theophylline
- Rarely used due to narrow therapeutic window and side effects
- Mentioned in GINA for resource-limited settings but largely obsolete
Optimizing Therapy
- Proper inhaler technique and use of spacers improve efficacy
- Adjust ICS dose based on symptoms and side effects
Nonpharmacologic Measures
- Weight management improves asthma control
- Encourage exercise, reframe as "asthma with exertional trigger"
- Identify and avoid triggers
- Refer to pulmonary rehabilitation
- Symptom journaling helps track patterns
- Stay up to date on vaccines (influenza, RSV, COVID-19, pneumonia)
Asthma Exacerbations
PEF and Asthma Action Plans
- Establish a baseline PEF to monitor exacerbations
- Green: 100-80%, well-controlled
- Yellow: 50-80%, increase meds, consider systemic steroids
- Red: <50%, urgent treatment, possible ED visit
Emergency Department Criteria
- Speaking in short sentences (4-5 words)
- Severe respiratory distress
- Rule out alternative diagnoses like CHF or infections
Azithromycin
- May reduce exacerbations in severe asthma
- Potential benefit for eosinophilic and noneosinophilic asthma
Persistent Asthma Symptoms
Specialist Referral
- Early referral for severe, uncontrolled, or complex asthma
- Consider referral for biologic therapy assessment
Comprehensive Workup
- CBC with eosinophils, high-resolution CT
- Rule out mimickers: pro-BNP, ANCA, echocardiography
Asthma Phenotypes
- High T2 Inflammation: Allergic asthma, high eosinophils, responds to ICS and biologics
- Low T2 Asthma: Poor response to biologics, limited treatment options
- Cough-variant Asthma: Montelukast may help
- Obesity-associated Asthma: Unique pathophysiology, often harder to control
