ACID-BASE

Metabolic or Respiratory problem?
Metabolic problems involve change in serum bicarb or anion gap
Respiratory problems involve change in PCO2
Diagnostic approach to metabolic pH abnormalities
- Determine the anion gap
- If AG is normal, look at bicarb
- Bicarb<22: Pure NAGMA
- Bicarb>28: Pure metabolic alkalosis
- Bicarb 22-28: Normal pH status
- If HIGH anion gap, determine the delta-delta
- Delta anion gap = (Anion Gap) – 10. This is roughly the degree of elevation of the anion gap.
- Delta bicarbonate = 24 – bicarbonate. This is roughly the degree of reduction of the serum bicarbonate.
- If ΔAG ~ ΔBicarb--> Pure AGMA
- If ΔAG > ΔBicarb--> AGMA + metabolic alkalosis
- If ΔAG < ΔBicarb--> Combined AGMA + NAGMA
Metabolic Acidosis
High Anion Gap (AGMA)
Anion Gap (AG) = Na – Bicarb – Chloride
- Normal is 4-12mM
Anion Gap
- Compare the AG to baseline (i.e. patients with chronic renal failure may have chronically elevated anion gap)
- No need to correct for albumin
Causes of AGMA
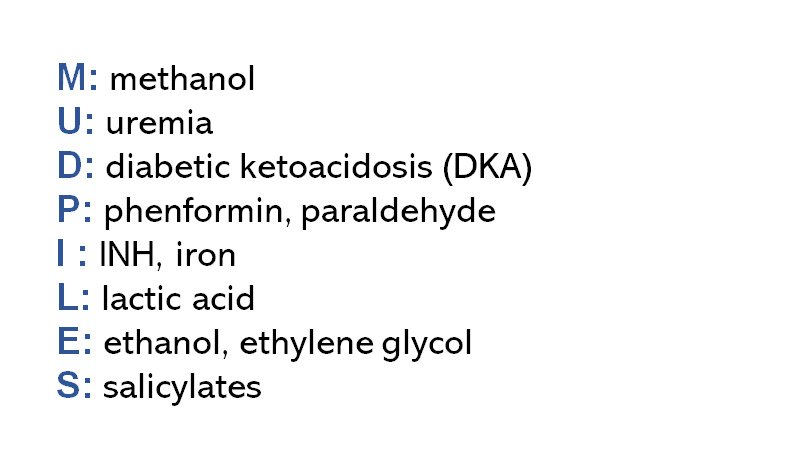
- Ketoacidosis: DKA, alcoholic ketoacidosis, starvation ketoacidosis
- Uremic acidosis: when GFR<30
- Lactic acidosis
- Inadequate oxygen delivery: shock, ischemia, muscle hyperactivity (seizure), extreme anemia
- Adequate oxygen delivery: liver failure, malignancy, thiamine deficiency, exogenous epinephrine/albuterol, endogenous epinephrine (shock), lactic alkalosis, severe DKA
- Medications: NSAIDs, epinephrine, albuterol, metformin, linezolid, HIV drugs, propofol, propylene glycol intoxication (usually due to high IV doses of lorazepam, diazepam, nitro, esmolol, phenytoin), nitroprusside, valproate/topiramate
- Poisoning: Acetaminophen, alcohols (ethylene glycol, methanol, ethanol), cyanide, carbon monoxide, salicylate, cocaine/amphetamines, iron
- Others: Hyperphosphatemia, metabolic alkalosis, D-hyperlactatemia (rare, due to bacterial fermenation follow small bowel resection)
Evaluate cause of AGMA
- Check CBC: Elevated WBC count of increase neutrophil/lymphocyte ratio may represent systemic illness/ sepsis
- Repeat electrolytes including Ca/Mg/Phos
- Check LFT's: liver disease may cause elevated lactate levels
- Lactate level
- Beta-hydroxybutyrate level (more accurate than urinary ketones)
- Evaluate for poisonings- salicylates, acetaminophen, carbon monoxide, toxic alcohols
- Consider differential diagnosis (above), review medications
- Calculate Delta-Delta
Delta-Delta
Exam
Look for signs of shock (tachycardia, low urine output, hypotension, confusion) and signs of ischemia (abdominal pain, cold limbs)
Treatment of AGMA
- Treat identifiable causes
- Empiric IV thiamine 200mg IV q12h: thiamine deficiency much more common than we think and impossible to accurately test for
- Bicarbonate: really only useful in uremic AGMA, not helpful in lactic acidosis, DKA regardless of pH
- Dialysis: For patients with acidosis + renal failure especially if volume overloaded
- Indicated if pH <7.15 despite treatment or in specific intoxications (metformin, ethylene glycol, methanol, salicylate)
BEWARE, AG isn't reliable in detecting mild degrees of lactic acidosis (lactate of 2-4mM). Normal anion gap has a wide range, so someone with a baseline anion gap that is low (~4mM) can develop a lactic acidosis yet have a normal AG
How does ABG/VBG help?
Provides info about respiratory pH abnormalities. Answers 2 main questions
- Is there adequate respiratory compensation?--> Metabolic alkalosis may be compensated for by mild hypoventilation & metabolic acidosis may be compensated for by hyperventilation
- Is there a primary respiratory disorder? / Is this pH abnormality due to a secondary compensatory response to a respiratory abnormality?
- Metabolic acidosis could be due to a chronic respiratory alkalosis (extremely rare unless patient is mismanaged on a mechanical vent)
- Metabolic alkalosis could be due to a chronic respiratory acidosis (common in hypercapnic patients, esp. in COPD, obesity hypoventilation syndrome, chronic opioids)
Winters' Formula
To determine other forms of compensation, it is not necessary to remember all of the different formulas and to instead just use a cheat sheet:
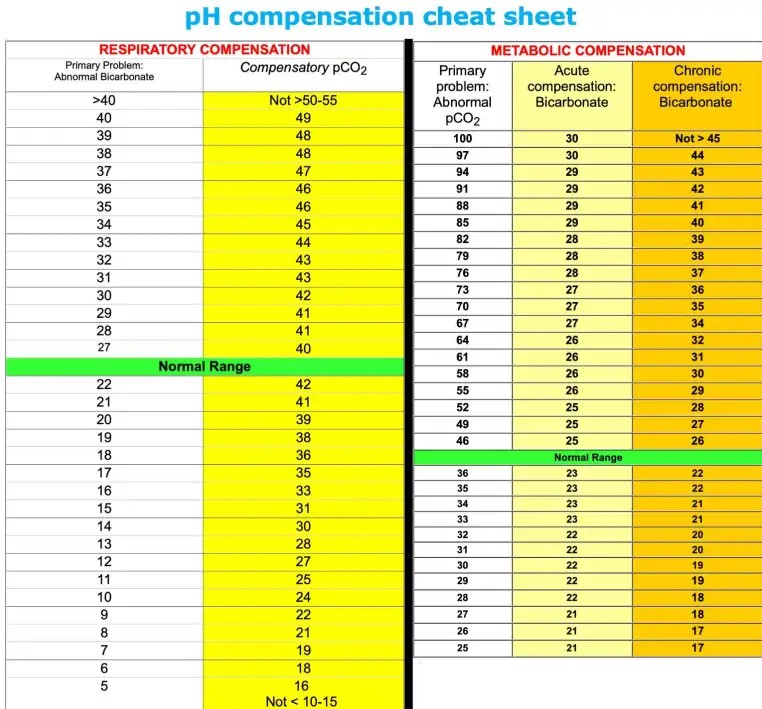
Cheat sheet for metabolic and respiratory compensation
Normal Anion Gap Metabolic Acidosis (NAGMA)
- Patient with normal anion gap with metabolic acidosis + Bicarb < 22
- Patient with anion gap metabolic acidosis, but the decrease in bicarb > elevation in anion gap (combined AGMA+NAGMA)
Causes of NAGMA
- Normal saline infusion
- Resolving DKA
- GI bicarb losses: Diarrhea, fistula, pancreatic/biliary drainage
- Renal insufficiency if GFR btwn 20-50
- Exogenous acids: TPN, calcium chloride
- Chronic hyperventilation (very rare)
- RTA
Workup for NAGMA
- Cause is usually obvious based on history and medications
- Look at potassium level, can be early clue
- High/normal potassium--> NS infusion, TPN, RTA type-4, chronic renal insufficiency
- Low potassium: GI losses, RTA-type1/2
- Check electrolytes (including Ca/Mg/Phos)
- Check UA
- Check urine chemistries
- Urine: pH, sodium, potassium, glucose, urea, osmolarity
- Calculate urine osmolar gap to diagnose type 1 or type 4 RTA--> indirect measurement of ammonium (acid) excretion by kidney
- Osmolar Gap = Urine osmolarity – 2(sodium + potassium) – Glucose(in mg/dL)/18 – Urea(in mg/dL)/28
- Osmolar gap >150 mOsm: appropriate ammonium excretion (excluding RTA type I or IV)
- Osmolar gap <150 mOsm: inadequate ammonium excretion (suggests RTA type I or IV)
- Type II RTA may secrete normal amounts of ammonium (and thus their urine osmolar gap may be appropriately elevated)
- Osmolar Gap = Urine osmolarity – 2(sodium + potassium) – Glucose(in mg/dL)/18 – Urea(in mg/dL)/28
Urine Osmolar Gap
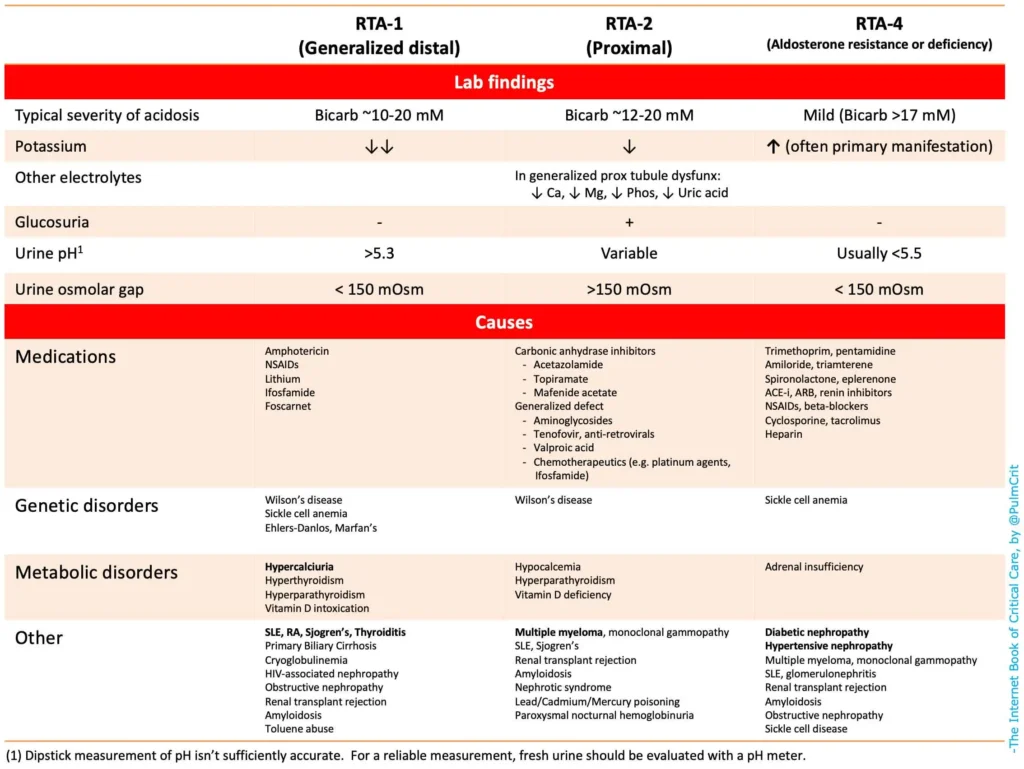
RTA Class
Type-4 RTA
- Caused by impaired renin secretion (diabetes, htn, glomerulonephritis, NSAIDs, beta blockers)
- Caused by impaired aldosterone production (adrenal insufficiency, critical illness, heparin, ACEI/ARBs, renin inhibitors)
- Caused by kidney being refractory to aldosterone (SLE, amyloid, obstructive uropathy, K+ sparing diuretics etc.)
Treatment of NAGMA
- Treat underlying cause (medication, give fludrocortisone if type-4 RTA)
- It is controversial whether NAGMA requires treatment, some rationale to treat include: hyperchloremic acidosis can injure kidneys/cause systemic inflammation, acidosis increases work of breathing (by compensatory respiratory alkalosis), acidosis increases insulin resistance
- 2 indications for treatment: Bicarb < 18, OR patient is at increased risk of harm from acidosis (AKI, DKA)
- NAGMA represents an imbalance between sodium chloride and sodium bicarb, so treatment involves adding sodium bicarb and removing sodium bicarb. Treatment however depends on volume status. The optimal treatment will simultaneously address the NAGMA, the volume status, and the sodium concentration.
- Hypovolemia –> Add sodium bicarbonate.
- Euvolemia –> Add sodium bicarbonate and remove sodium chloride simultaneously. The goal here is to replace bicarbonate with chloride, without shifting the volume status.
- Hypervolemia –> Remove sodium chloride via diuresis.
- If repleting bicarb, calculate the patient's bicarbonate deficit
Bicarbonate Deficit Calculator
Reduced anion gap
- MOST COMMONLY just a lab error due to hypernatremia, hyperlipidemia
- 1st step is to recheck it
- Some other causes can be increased levels of cations (hyperkalemia, hypercalcemia), lithium toxicity, multiple myeloma
Metabolic Alkalosis
- Symptoms: seizures (typically at Bicarb>50), delirium, arrhythmia, hypocalcemia (high pH causes calcium to bind albumin), hypoventilation (respiratory compensation)
- Causes
- Compensation for chronic respiratory acidosis- COPD, obesity hypoventilation, respiratory muscle weakness
- Chloride- depletion metabolic alkalosis- vomiting, NG suction, chloride-wasting diarrhea (laxative abuse), diuresis, renal hypoperfusion + exogenous alkali (i.e. patient with CHF takes a lot of TUMS)
- Non-chloride depletion metabolic alkalosis- thiazide/loop diuretics, hypomagnesemia/hypokalemia, hypoaldosteronism, renal insufficiency + exogenous alkali (i.e. patient with kidney failure takes a lot of TUMS)
Workup for Metabolic Alkalosis
- History, physical: Usually reveals the cause.
- If hypovolemic based on history/ bedisde echo--> chloride deficiency
- Hypertension suggest excess aldosterone
- Chronicity (i.e. chronic metabolic alkalosis suggest chronic compensation for COPD)
- Labs, including Ca/Mg/Phos, ABG/VBG to evaluate if it's compensatory metabolic alkalosis
- Urine potassium and urine chloride levels
- Urine potassium <20-30 mM: hypokalemia may be contributory
- Urine chloride concentration is the most important:
- Chloride <10-30 mM: suggests saline responsive.
- Chloride >10-30 mM: suggests saline unresponsive.
- Chloride between 10-30 mM: gray area
- Evaluate RAAS (usually unnecessary). May consider if patient has persistent alkalosis with high urine chloride and is refractory to NS infusion or if other signs of excess RAAS (hypertension, hyperkalemia)
- Measure serum renin and aldosterone levels
- ↓ renin & ↑ aldosterone: Primary hyperaldosteronism (aldosterone-secreting adenoma, bilateral adrenal hyperplasia).
- ↑ renin & ↑ high aldosterone: Secondary hyperaldosteronism (renin-secreting tumor, renal artery stenosis).
- ↓ renin & ↓ aldosterone: State of apparent mineralocorticoid excess (Cushing syndrome, exogenous mineralocorticoid, licorice ingestion).
- Measure serum renin and aldosterone levels
When NOT to treat a metabolic alkalosis?
- Compensatory metabolic alkalosis due to respiratory acidosis: Do not treat, their compensatory mechanism is beneficial, metabolic alkalosis allows them to have a normal pH despite hypoventilation
When TO treat a metabolic alkalosis?
- Usually the goal is to treat the underlying cause (i.e. patient is hypovolemic, give them fluids). Treatment may be indicated in following circumstances:
- Alkalosis is severe/symptomatic
- Process causing alkalosis isn't easily reversed (most commonly patient being diuresed develops contraction alkalosis but needs to keep being diuresed)
Treatment for Metabolic Alkalosis
- Give potassium chloride target K>4.5: Hypokalemia maintains alkalosis
- Give magnesium: hypomagnesemia contributes to alkalosis and makes it harder to tx the hypokalemia
- Give normal saline if hypovolemic: if urine chloride < 10-30 then they are saline responsive. Acidotic NS preferred over LR
- Give diuretics (ACETAZOLAMIDE) if hypervolemic: Acetozolamide will cause bicarb excretion (ensure to monitor potassium, can make hypokalemic which worsens the alkalosis).
- Spironolactone is 2nd line, but can take 24-48h to work
- Hold/ decrease the dose of alkalosis-inducing diuretics (furosemide): If euvolemic you can discontinue, if still volume overloaded can give furosemide + acetazolamide
- Give a PPI if ongoing vomiting/ NG suction: loss of gastric acid will cause metabolic alkalosis, PPI neutralizes the pH preventing loss of acid
- Dialysis: rarely needed in metabolic alkalosis unless profound electrolyte abnormalities
- IV HCl: last resort if all else fails (and pH >7.55 or bicarb> 38). Must be given via central line
Primary Respiratory Pathologies
Respiratory Acidosis
Symptoms
- Delirium, somnolence, coma, tremor, asterixis, headache (upon wakening in nocturnal hypoventilation)
- If chronic, patient's adapt and may present with only somnolence
Lab diagnosis- based on ABG/VBG
- PaCO2 > 45
- Primary hypercapnia: isn't a compensatory response to metabolic alkalosis
- Look at baseline bicarbonate level. In chronic hypercapnia, there will be a greater degree of compensatory metabolic alkalosis
Causes of hypercapnia
- Won't breathe: medications like opioids, benzos, alcohol, brainstem dysfunction (trauma, stroke, tumor), hypothyroid
- Can't breathe: spinal cord problem (C3-C5 injury), MS/transverse myeleitis, tumor, neuromuscular disorders (GBS, ALS, MG etc.), restricted lung inflation (abdominal compartment syndrome, obesity hypoventilation, pleural effusion, kyphosis etc.), upper airway problem (angioedema, foreign body etc.), lower airway problem (COPD/asthma)
- Breathing isn't working: alveolar disease (pneumonia, ARDS, ILD) or vascular disease (PE)
Evaluation
- Physical exam: if low RR think opioids/ CNS issue, if not distressed then think chronic problem or neuro issue, neurologic exam to look at brainstem/spinal cord issue, auscultate to look for signs of bronchospasm, stridor, air movement
- Labs: electrolytes (including Ca/Mg/Phos), TSH, CBC (polycythemia= chronic hypoxia), CK (to look for myopathies, hypothyroid), look at pH/bicarbonate
- Imaging: CXR, MRI of brain spine if suspicious for neurologic problem, CT neck/lungs, CTA
Consequences of hypercapnia
- Generally tolerated well, chronic COPD patients live many years with high CO2 and the hypercapnia itself is not harmful
- Permissive hypercapnia: allow CO2 to increase on vent to avoid barotrauma
- Potential risks: dyspnea with agitation (bucking the ventilator), sedation (CO2 narcosis), pulmonary vasoconstriction (can be bad in patient with pulmonary htn), increased ICP (vasodilate cerebral arteries)
Treatment- No universal approach, causes vary. If patient is chronically hypercapnic, goal is to return to baseline
- Hypercapnia due to opioid intoxication may involve naloxone
- Hypercapnia due to neuromuscular weakness may often be improved with noninvasive ventilation
- Hypercapnia due to asthma or COPD requires specific treatment pathways
- Mild-moderate hypercapnia in an intubated patient may often be monitored without intervention (permissive hypercapnia).
Respiratory Alkalosis
- Hypocapnia is by far the most common acid-base disorder in sick patients
Diagnosis- based on ABG/VBG
- pCO2 < 35mm
Symptoms
- Anxiety, delirium, seizure, sx of hypocalcemia (since alkalemia reduces ionized calcium levels) such as paresthesias/cramps, arrhythmia
Causes
- Nearly any pulmonary disease: pneumonia, asthma, pulmonary embolism, pneumothorax, mechanical ventilation
- Neurologic: pain, anxiety, meningitis/encephalitis, trauma, stroke
- Medications: salicylates, topiramate, caffeine, nicotine, beta-agonists, progesterone
- Endocrine: thyrotoxicosis, pregnancy
- Cirrhosis
- Sepsis (early sign that can precede hypoxemia/ hypotension)
Workup
- Cause is often evident from history and physical, if unclear some of the following may be considered:
- Salicylate level, TSH, LFT's, beta-HCG, PE eval (D-dimer, CTA), sepsis eval, neuroimaging
Consequences of hypocapnia
- Cerebral vasoconstriction which causes hypoperfusion
- Suppression of respiratory drive, bronchoconstriction
- Can cause a lactic alkalosis
Treatment
- Treat the identifiable etiology, often involves properly treating pain and ensuring sedation if appropriate
- If ventilated: reduce the TV or RR
